HELLP Syndrome
RyanKings999

Written by Mindsmaking Medical Writer
Fact Checked by Mindsmaking Professionals
11th, June, 2025
HELLP syndrome is a serious pregnancy complication affecting the liver and blood. Symptoms like nausea, swelling, or unusual bleeding should be taken seriously. What causes HELLP and how can it be safely managed for mom and baby?
HELLP syndrome is a rare pregnancy complication that mainly affects the blood and liver. It often occurs during the third trimester of pregnancy, between 28 to 37 weeks, but can occur anytime in the second half of pregnancy. HELLP syndrome can also develop after childbirth. (5)
It is a serious pregnancy complication that can be life-threatening to both mother and baby if not identified early. It presents with symptoms like those of preeclampsia, which include high blood pressure, swelling in the legs, and protein in the urine.( 7)
So recognizing these symptoms on time is important to prevent severe complications, including liver damage, bleeding, or worse, death
In some cases, HELLP Syndrome goes away on its own after delivery, but treatment can help resolve symptoms. Because it can be life-threatening, regular prenatal checkups are important to ensure the health of both mom and baby.
Key Takeaways
HELLP syndrome is a pregnancy complication that mainly affects your blood and liver. It often occurs during the third trimester between 28 to 37 weeks.
HELLP Syndrome is known for the breakdown of red blood cells (hemolysis), elevated liver enzymes, and a low platelet count.
Possible causes and risk factors associated with the HELLP Syndrome include: being of older maternal age, of a Caucasian or European descent, and having a history of preeclampsia or eclampsia.
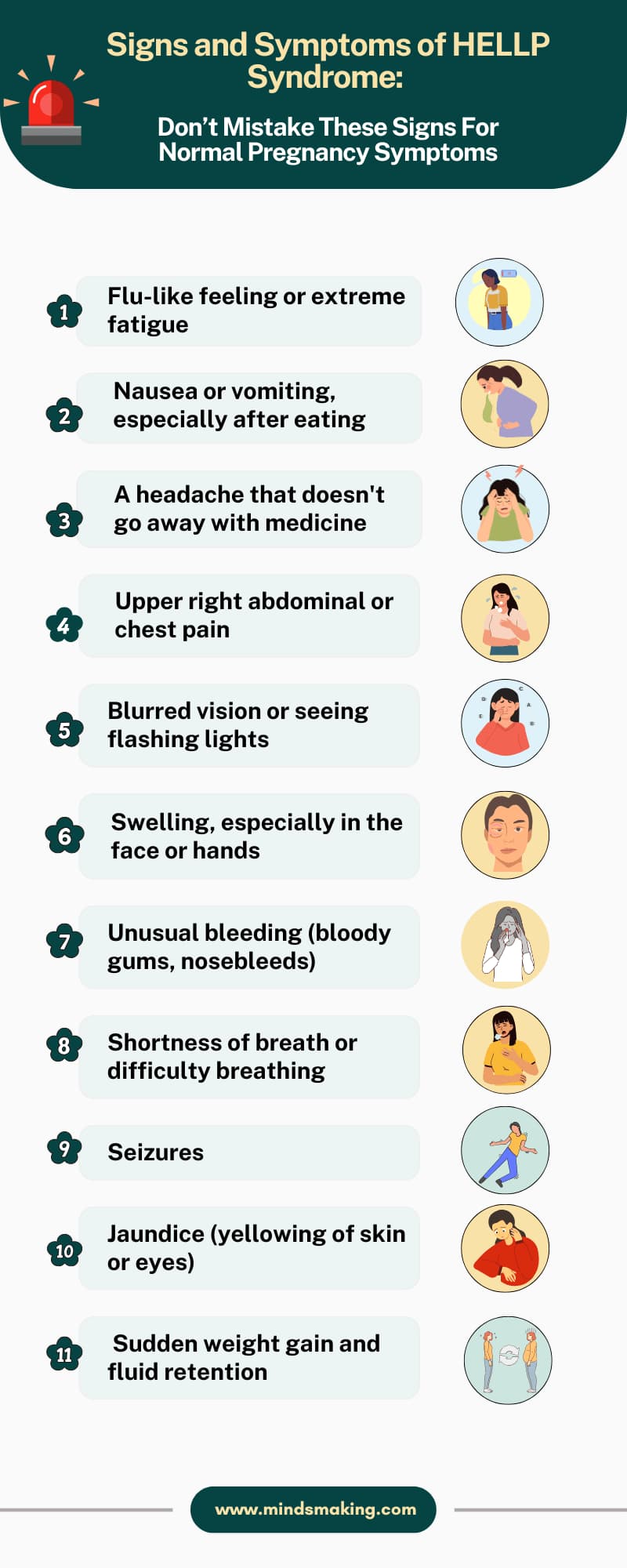
Symptoms of HELLP syndrome are: flu-like feeling, nausea and vomiting, abdominal or chest pain, swelling especially of the face and hands, edema, and jaundice.
For HELLP syndrome to be diagnosed, there are combinations of clinical symptoms and laboratory tests that would be carried out.
HELLP syndrome is treated by first making sure the mom is stable and checking how the baby is doing, then delivering the baby if things get worse quickly.
To increase your chances of a healthy pregnancy, eat nutrient-packed food, exercise often, sleep at least 8 hours, and always go for prenatal checkups.
What is HELLP Syndrome?
HELLP syndrome is a serious complication that can occur during pregnancy. It is known for the breakdown of red blood cells (hemolysis), elevated liver enzymes, and a low platelet count. (6)
While it is usually linked to preeclampsia, it can happen on its own. This condition comes with significant risks for both you and your baby, making immediate medical care important.
The acronym for HELLP stands for:
- H - hemolysis, which is the breaking down of red blood cells, which can lead to anemia or other complications
- EL - elevated liver enzymes, a sign that the liver may be damaged.
- LP - low platelet count, platelets help blood to clot, so having low levels increases the risk of bleeding
This syndrome occurs in about 0.5% to 0.9% of all pregnancies and in 10% to 20% of cases of severe preeclampsia. It can cause severe complications for the mother and fetus, including Liver rupture or hematoma, kidney failure, pulmonary edema, placental abruption, and preterm birth. (6)
HELLP syndrome is closely related to preeclampsia, which is a hypertensive disorder in pregnancy with symptoms such as high blood pressure and proteinuria. In fact, HELLP is considered by many clinicians as a severe form or complication of preeclampsia.
But their relationship is not really clear because about 10–20% of HELLP cases occur without high blood pressure or proteinuria, which suggests that while they may be related, HELLP syndrome can occur without these symptoms. (6)
Some experts also argue that HELLP is a separate condition with its own diagnosis and management, but it often coexists with preeclampsia.
Early detection and diagnosis are important because serious illness and even death can occur in about 25% of cases. As a result, being aware of HELLP syndrome and how it relates to preeclampsia is helpful to ensure the best medical care for you and your baby. (6)
Causes of HELLP Syndrome
Professor Kristin Beach, a Registered nurse, shares with us that when you have preeclampsia, which is a form of hypertension that is not chronic that develops particularly during the third trimester of pregnancy, you can get a form of HELLP syndrome.
There are other possible causes and risk factors associated with the development of HELLP Syndrome.
- If you have had a history of HELLP syndrome in your previous pregnancy, then you are at risk of still developing it.
- If you have been diagnosed with preeclampsia or eclampsia because up to 1 in 5 people who have these two conditions will develop HELLP syndrome. (3)
- If you are of Caucasian or European descent.
- If you are of older maternal age between 25 to 35.
- If you have a pre-existing condition such as chronic hypertension, kidney disease, or diabetes.
You may have a higher chance of developing HELLP syndrome because of the genes you inherit from your parents and how your immune system behaves during pregnancy.
Studies suggest a genetic component to HELLP syndrome, with women having a family history or previous HELLP pregnancies at higher risk. Specific genetic variations, like those in TLR4 and NOD2 genes, have also been linked to impaired innate immune responses and increased susceptibility to early-onset preeclampsia and HELLP syndrome. (1)
Research shows a genetic component to HELLP syndrome. The differences in genes related to immune function and inflammation may predispose you to this condition. (1)
The hypertension associated with preeclampsia can lead to endothelial damage and impaired blood flow, contributing to the development of HELLP. Elevated blood pressure can cause stress on your liver and blood vessels, leading to hemolysis, elevated liver enzymes, and low platelet count, which is HELLP syndrome.
What are the Symptoms of HELLP Syndrome
According to the National Institute of Health, patients with HELLP syndrome may present with severe bleeding, jaundice, vomiting, and fatigue. (5)
Also, Professor Kristin Beach, a Registered nurse, shares one and the most serious signs of all, which is bleeding. This is not particularly vaginal bleeding but irregular bleeding for example spontaneous nosebleeds or bloody gums which could occur due to low platelet count. This spontaneous bleeding can be dangerous during pregnancy.
HELLP syndrome often presents with symptoms that mimic other conditions, and if not caught on time, can be fatal.(8)(6)
These early warning signs include:
- Flu-like feeling
- Fatigue or weakness
- Nausea, vomiting, or indigestion with pain after eating
- A headache that won't go away, even after taking medication such as acetaminophen
- Abdominal or chest pain, including abdominal or chest tenderness and upper right side pain from liver distention
- Swelling, especially of the face or hands
Severe Symptoms include:
- Changes in vision, including blurred vision, seeing double, or flashing lights or auras
- Shortness of breath, difficult breathing, or gasping for air
- Seizures, most especially if HELLP has progressed to eclampsia
- Jaundice, which is the yellowing of the skin or eyes due to liver dysfunction
- Fluid retention (edema) and excess weight gain
The Symptoms of HELLP syndrome often mimic other, more common conditions during pregnancy, and misdiagnoses could occur. Acute fatty liver of pregnancy (AFLP), which develops in the third trimester and often presents with symptoms like general malaise, loss of appetite, nausea and vomiting, right upper abdominal pain, headaches, and jaundice, which are the same as those of HELLP syndrome. (6)
This is why regular prenatal checkups and seeing your doctor if any of the symptoms present themselves are important.
mindsmakin
Read This Next
No posts available
How is HELLP Syndrome Diagnosed?
For HELLP syndrome to be diagnosed, there are combinations of clinical symptoms and laboratory tests that would be carried out by the doctor.(12)
The process can be urgent and can progress quickly, especially if you have already started experiencing symptoms like headaches, blurry vision, or abdominal and upper right side pain when in your third trimester or even postpartum.
Stephanie Patch, a Clovis mom diagnosed with HELLP syndrome, recounted her experience. She was in her third trimester when, all of a sudden, she felt severe upper abdominal pain and was rushed to the hospital.
Her liver started failing, her platelets dropped, and she was taken straight to the operating theater for delivery. Stephanie’s experience shows how quickly the symptoms can progress.
First, your doctor would run a blood test (Complete Blood Count) to assess your overall blood health, focusing mainly on Hemoglobin, Hemocrit, and platelet count, which may all be low due to the breakdown of red blood cells leading to hemolysis. Your platelet count is typically reduced to below 100,000 as a result of red blood cell breakdown and hemolysis.
Secondly, a Liver function test (LFTs) would be carried out to check how well your liver is functioning. The test will focus on your AST and ALT, LDH, and bilirubin, to check if they are all elevated.
Next is your electrolytes, if they are balanced and will be assessed for any kidney or metabolic complications.
You will also be screened to determine your blood type and RH factor in case a blood transfusion is needed if your hemoglobin drops or bleeding occurs.
Lastly, an imaging will be performed on you. This is to rule out any form of cerebral edema or stroke. But if you present with a seizure or blurring vision, it would be needed to check for bleeding or swelling.
How is HELLP Syndrome Treated
In the treatment of HELLP syndrome, the most definite outcome is the delivery of the baby. But before this, the mother will be stabilized, the baby's status will be assessed, and then immediate delivery will be performed if the symptoms progress quickly. This was explained by Kristin Bear, a registered nurse.(6)
- Your doctor will focus on stabilizing you and checking your blood pressure, oxygen levels, and overall condition. They'll also monitor your baby with a nonstress test and ultrasound to see how they're doing.
- To regulate your blood pressure, you will be given medications like labetalol, hydralazine and nifedipine
- If you are having severe upper belly pain or your liver tests are off, you will have an imaging (like an ultrasound, CT, or MRI) to check for things like liver bleeding, rupture, and liver failure.
- In serious cases, surgery or even a liver transplant might be needed. If you're stable, a less invasive option like artery embolization could be considered.
- If your platelet count drops too low, you might need blood transfusions, platelets if you’re bleeding, plasma, or cryoprecipitate if your blood is not clotting well. If you have a rare condition called TTP alongside HELLP, you’ll likely need plasma exchange.
- If your lungs and kidneys are affected, you will be on oxygen or a ventilator, IV fluids or dialysis, and close monitoring in the ICU.
- Once you are stable, your doctors will focus on delivering your baby. If you are less than 34 weeks pregnant, you will be given betamethasone to help your baby’s lungs mature. You will also be started on magnesium sulfate to prevent seizures and protect your baby’s brain.(5)
How to Prevent HELLP Syndrome
According to the American Pregnancy Association, there is no known definite cause for HELLP Syndrome, and so there is no way to prevent it. But getting regular prenatal care is the best thing you can do to reduce your risk of most pregnancy complications.(2)
If you are at high risk of developing HELLP syndrome, your doctor may recommend that you take a low-dose aspirin after your first trimester.
Here are other things you can do to increase your chances of having a healthy pregnancy.
- Always prioritize eating nutrient-packed foods like fruits, vegetables, lean protein, and whole grains.
- Always be physically active. The World Health Organization recommends at least 150 minutes of moderate-intensity physical activity per week.
- Sleep. Let this be among your priorities. Have at least 8 hours of sleep.
- Never miss any of your prenatal visits and checkups.
Early screening and monitoring during pregnancy, including blood tests and ultrasounds, play an important role in managing HELLP syndrome, a severe complication of preeclampsia. While there's no known way to entirely prevent HELLP, regular prenatal care allows for early detection and treatment, which can improve maternal and fetal outcomes.(3)
mindsmaking

Frequently Asked Questions
When does HELLP syndrome usually occur?
HELLP syndrome often occurs during the third trimester of pregnancy, between 28 to 37 weeks, but can occur anytime in the second half of pregnancy. It can also develop 48 hours after childbirth.
Is HELLP syndrome life-threatening?
Yes, it is a life-threatening pregnancy complication that, if it is not identified and treated on time, can progress and lead to more severe complications such as liver damage, placental abruption, or worse, death.
How soon after delivery does HELLP syndrome resolve?
After your baby is born, HELLP syndrome usually goes away within a few days.
Can HELLP syndrome happen twice?
Yes, if you have had HELLP syndrome in your previous pregnancy, you are at a higher risk of developing it again in your subsequent pregnancies.
What is the survival rate for HELLP syndrome?
The mortality rate of women with HELLP syndrome is 0%-24%, with a perinatal death rate of up to 37%. (5)
Can HELLP syndrome be detected in early pregnancy?
Yes. HELLP syndrome can occur anytime during the second half of pregnancy. The occurrence of HELLP syndrome diagnosed before the 20th week of gestation has been most commonly reported in association with antiphospholipid antibody syndrome (APS) or triploid chromosomal anomalies.
Is HELLP syndrome the same as preeclampsia?
HELLP syndrome is often considered a severe form of preeclampsia, but some experts consider it a disease on its own. This is because some HELLP syndrome diagnoses don't always come with hypertension or proteinuria
Can HELLP syndrome affect the baby?
The effects of HELLP syndrome on your baby can vary depending on your baby's gestational age, his/her weight at delivery, and any complications that may arise from their early delivery. If your baby weighs at least 2 pounds at birth, he or she has the same survival rate and health outcome as non-HELLP babies of the same size.
Is HELLP syndrome preventable?
While there is no known way to prevent HELLP syndrome, maintaining a healthy lifestyle before and during your pregnancy, attending regular prenatal checkups, exercising, and eating nutrient-packed food can help reduce your likelihood of developing the syndrome.
Was this article helpful?
How many stars are you giving this article?
Leave a comment
Your email address will not be published.









































