Anemia In Pregnancy
Getty images

Written by Mindsmaking Medical Writer
Fact Checked by Mindsmaking Professionals
2nd, June, 2025
Anemia in pregnancy is a serious health issue that can affect both mother and baby if left untreated. Early diagnosis and proper treatment are essential to reduce the risk of complications.
Anemia during pregnancy is a common yet serious condition that can significantly impact the health of both the mother and baby. It happens when the body does not have enough healthy red blood cells to carry adequate oxygen to the tissues and the growing fetus. If left untreated, anemia can lead to complications such as premature birth, low birth weight, and postpartum depression. (12)
Anemia affects nearly 37% of all pregnancies worldwide, according to the World Health Organization (WHO) (23). Iron deficiency is the most common cause of anemia during pregnancy, but folate and vitamin B12 deficiencies can also contribute to anemia.
Symptoms like fatigue, shortness of breath, dizziness, and pale skin are often overlooked as normal pregnancy discomforts, which is why awareness and regular screening are important.(6)
The good news is that anemia during pregnancy is highly treatable. Eating iron-rich foods, taking the right supplements, and getting regular check-ups can help keep you and your baby healthy. In some cases, doctors may give stronger treatments if needed. With the right care, anemia can be managed, and you can have a safe and healthy pregnancy.
Key Takeaways
Anemia in pregnancy is defined as having hemoglobin levels below 11 g/dL. The most common form is iron-deficiency anemia, but folate and vitamin B12 deficiencies also play major roles and can lead to developmental risks.
Anemia affects nearly 37% of all pregnancies worldwide.
Iron and vitamin deficiencies, poor dietary intake, blood loss, infections like malaria or HIV, and inherited blood disorders such as thalassemia and sickle cell disease cause anemia.
During pregnancy, blood volume increases by about 20 to 30% to support fetal development. This increases the supply of iron and vitamins that the body needs to make hemoglobin.
Common symptoms of anemia include tiredness, pale skin, dizziness, and shortness of breath. Severe cases may show rapid heartbeat, low blood pressure, and difficulty concentrating, though many symptoms overlap with normal pregnancy discomforts.
Anemia if left untreated, can lead to premature birth, low birth weight, stillbirth, and intrauterine growth restriction.
Preventing anemia includes eating an iron- and folate-rich diet, taking prenatal vitamins, avoiding calcium-rich foods around iron intake, and attending regular antenatal checkups.
What is Anemia During Pregnancy?
The World Health Organization defines anemia in pregnancy as having a hemoglobin level lower than 11 g/dL. (9)
Anemia during pregnancy happens when the body does not have enough healthy red blood cells or hemoglobin to carry oxygen to the body and the growing baby. Without enough hemoglobin, the body and baby may not get the oxygen they need to stay healthy. (23)
Hemoglobin is the iron-rich protein in red blood cells that helps move oxygen from the lungs to the rest of the body. During pregnancy, your blood volume increases by about 20 to 30% to support fetal development, which increases the supply of iron and vitamins that the body needs to make hemoglobin. (2)
This increased demand makes it important to maintain proper hemoglobin levels, which should be above 11 g/dL(19). When levels fall below this threshold, both mother and baby may face developmental concerns and heightened health risks for the mother.
Types of Anemia During Pregnancy
Several types of anemia can occur during pregnancy, and each has its own causes and risks.
Iron Deficiency Anemia: Iron deficiency anemia is the most common. It happens when insufficient iron is in your diet or your body can’t absorb it well. You may feel tired, look pale, or feel your heart beating faster.
Folate Deficiency Anemia: This is another common form caused by a low folate level. Folate is a type of vitamin B essential for cell growth and the production of red blood cells. Folate deficiency can also increase the risk of neural tube defects in babies.
Vitamin B12 Deficiency Anemia: Vitamin B12 deficiency anemia can happen if there is not enough animal products like meat, eggs, or milk in your diet. This vitamin helps your body make red blood cells and keeps your nerves healthy. This deficiency can lead to nerve damage and developmental problems if not treated. (13)
What Causes Anemia during Pregnancy?
Anemia during pregnancy can be caused by various factors, including nutrient deficiencies, inadequate diet or absorption of nutrients, infections, inflammation, chronic diseases, gynaecological and obstetric conditions, and inherited red blood cell disorders. (23) Rather than anemia being a disease itself, it is usually a sign of something else going on. Such as:
Iron Deficiency: During pregnancy, your body needs more iron to support you and your baby. If you don’t get enough iron from your diet or your body can’t absorb it properly, you may develop iron deficiency, the most common cause of anemia in pregnancy.
Vitamin Deficiencies: Your body needs key nutrients like folate (vitamin B9), vitamin B12, vitamin A, and riboflavin (vitamin B2) to produce healthy red blood cells. If you’re low on any of these, it can lead to anemia, and that can leave you feeling tired, dizzy, or short of breath.
Changes in Absorption or Diet: During pregnancy, your body goes through all sorts of changes. Sometimes, it doesn’t absorb nutrients as it used to or is supposed to. Health conditions, medications, or even how different nutrients interact with each other can affect how well your body takes in what you eat. So, even if you're eating well, your body might not be getting everything it needs.
Blood Loss: Blood loss can reduce the number of red blood cells in the body. This can happen due to heavy menstrual cycles before pregnancy, natural blood volume increasing during pregnancy, and blood loss during or after delivery, especially in cases of postpartum bleeding.
Infections: Certain infections, like hookworm or schistosomiasis, malaria, tuberculosis, and HIV, may affect nutrient absorption, increase blood loss, or impact how red blood cells are made or maintained.
Chronic Health Conditions: Long-term health conditions can lead to a type of anemia called anemia of chronic disease. In these cases, inflammation may affect how the body uses iron or produces red blood cells.
Inherited Blood Conditions: Anemia during pregnancy can be caused by inherited blood conditions, which are genetic disorders that affect the structure or function of red blood cells. One common example is thalassemia (both alpha and beta types), where the body does not produce red blood cells properly, leading to a shortage of healthy cells to carry oxygen. Another inherited condition is sickle cell disease, which causes red blood cells to become abnormally shaped, like a crescent or sickle, making it harder for them to flow smoothly through blood vessels and deliver oxygen efficiently.
Multiple pregnancy (e.g., twins): If you’re carrying more than one baby, such as in a twin pregnancy, your body has much more to take on, including a higher demand for iron and nutrients. If these nutritional needs aren’t adequately met, it can lead to anemia (7).
Back-to-back pregnancies: When pregnancies occur with little time in between, your body may not have enough time to fully recover or replenish essential nutrients like iron, folate, and vitamin B12, which increases the risk of anemia. This is particularly concerning in cases where there is a lack of proper postnatal nutrition or care after the first pregnancy (7).
The Risks Of Anemia During Pregnancy
Pregnancy demands more from your body. If your iron levels drop too low, it can lead to anemia, a condition where the blood can not carry enough oxygen to the tissues or the baby. While it might start with simple tiredness, untreated anemia during pregnancy can pose serious health risks for both mother and child.
Premature Birth (Preterm Delivery)
Babies are supposed to stay in the womb for about 9 months to develop fully. If the mother has anemia, the baby might be born too early, before 37 weeks. Premature babies often have underdeveloped organs, especially the lungs, and may need special care in the hospital to survive and grow. (20)
Low Birth Weight
Anemia reduces the amount of oxygen and nutrients reaching the baby. Without enough, the baby may not grow properly and may be born weighing less than 2.5 kg (about 5.5 pounds). Low birth weight can lead to more illnesses, trouble feeding, and a weaker immune system in the early months of life. (25)
Postpartum Depression
Having anemia during pregnancy can increase the risk of developing postpartum depression. Anemia, especially when caused by iron deficiency, can lead to feelings of extreme tiredness and low energy, which can affect your mood and mental health. Low iron levels can also impact brain function, making it harder to cope with the emotional challenges of pregnancy and motherhood (12).
Learning and behavioral issues
Anemia during pregnancy can increase the risk of learning and behavioral issues in children later on. This is because iron is essential for brain development; it helps form the structure of the brain, supports communication between brain cells, and ensures oxygen reaches developing tissues. When a mother doesn’t have enough iron, the baby may not get the oxygen and nutrients needed for healthy brain growth, which can affect memory, attention, and behavior as the child grows (4).
Stillbirth or Intrauterine Death
In severe cases of anemia, the baby may not get enough oxygen to survive. This can result in the baby dying in the womb before birth, also known as stillbirth. This risk is higher if the anemia is not diagnosed and treated early. (6)
Low APGAR Score at Birth
The appearance, pulse, grimace, activity, and respiration (APGAR) score checks a newborn’s health right after birth, including their breathing, heartbeat, and muscle tone. Babies born to anemic mothers often have lower scores, which may mean they need urgent medical attention right away to help them breathe or stay warm.
Intrauterine Growth Restriction (IUGR)
Occurs when a baby grows too slowly in the womb. One major cause can be anemia, which affects how well the placenta delivers oxygen and nutrients. If the placenta isn’t working efficiently, the baby may not get what it needs to grow properly. Babies affected by IUGR are more likely to face developmental delays and may be at higher risk of stunted growth during early childhood (9) (26).
Because of these possible problems, health experts like the American College of Obstetricians and Gynecologists (ACOG) recommend screening all pregnant people for anemia with a complete blood count twice during routine prenatal care: once in the first trimester and again between 24 weeks and 0 days gestation and 28 weeks and 6 days gestation. (5)
Even though there’s some disagreement among medical groups about whether everyone needs routine screening, many studies support the benefits.
Read This Next
No posts available
Symptoms of Anemia During Pregnancy
Early symptoms of anemia are often mild, nonspecific, or even nonexistent, making them easy to overlook. However, as the condition progresses, symptoms may become more noticeable and severe. Because some signs of anemia can be linked to other health issues, it’s important to consult your doctor for a proper diagnosis (24).
So, what symptoms should you look out for? Here are some of the most common signs:
Severe symptoms of Anemia
- A fast heartbeat.
- Low blood pressure. (17)
- Trouble concentrating. (17)
- Easily bruised. (23)
- Pale mucous membranes, especially in the mouth, nose, etc. (23)
mindsmaking

How is Anemia Diagnosed During Pregnancy?
If your doctor suspects anemia during pregnancy, often based on symptoms like fatigue or weakness, a blood test is required to confirm it. Anemia is typically diagnosed when hemoglobin (Hb) levels fall below 11 g/dL or hematocrit levels drop below 33% (10).
Doctors commonly evaluate red blood cell indices to diagnose iron deficiency anemia. Hemoglobin levels below 7 g/dL are considered severe and usually require urgent medical attention. Levels below 4 g/dL are critical and may become life-threatening, potentially leading to complications like heart failure, infections, or even death (10).
In such serious cases, especially when symptoms like chest pain, shortness of breath, or extreme fatigue are present, doctors may recommend a blood transfusion. This quickly boosts red blood cell levels and helps relieve symptoms. However, a transfusion is only temporary; iron supplements and further investigation are still needed to address the root cause (2).
Doctors typically begin the diagnosis with two main tests:
1. Complete Blood Count (CBC): This test measures levels of red blood cells, hemoglobin, and hematocrit. If hemoglobin levels fall below 11 g/dL in the first or third trimester, or below 10.5 g/dL in the second trimester, anemia may be diagnosed (14).
2. Mean Corpuscular Volume (MCV): This measures the size of red blood cells. If cells are smaller than normal (microcytic), doctors may check for iron deficiency using a serum ferritin test, or for genetic conditions like thalassemia using hemoglobin electrophoresis. If the red blood cells are larger than normal (macrocytic), vitamin B12 and folate levels will be tested. In cases where anemia has multiple causes, doctors may investigate both simultaneously (14).
Regular prenatal check-ups are key to detecting anemia early and ensuring effective treatments. Always inform your doctor of your feelings and report any side effects from supplements. If symptoms don’t improve, you may be referred to a hematologist or a maternal-fetal medicine specialist. Staying on top of your care is essential for your and your baby's health.
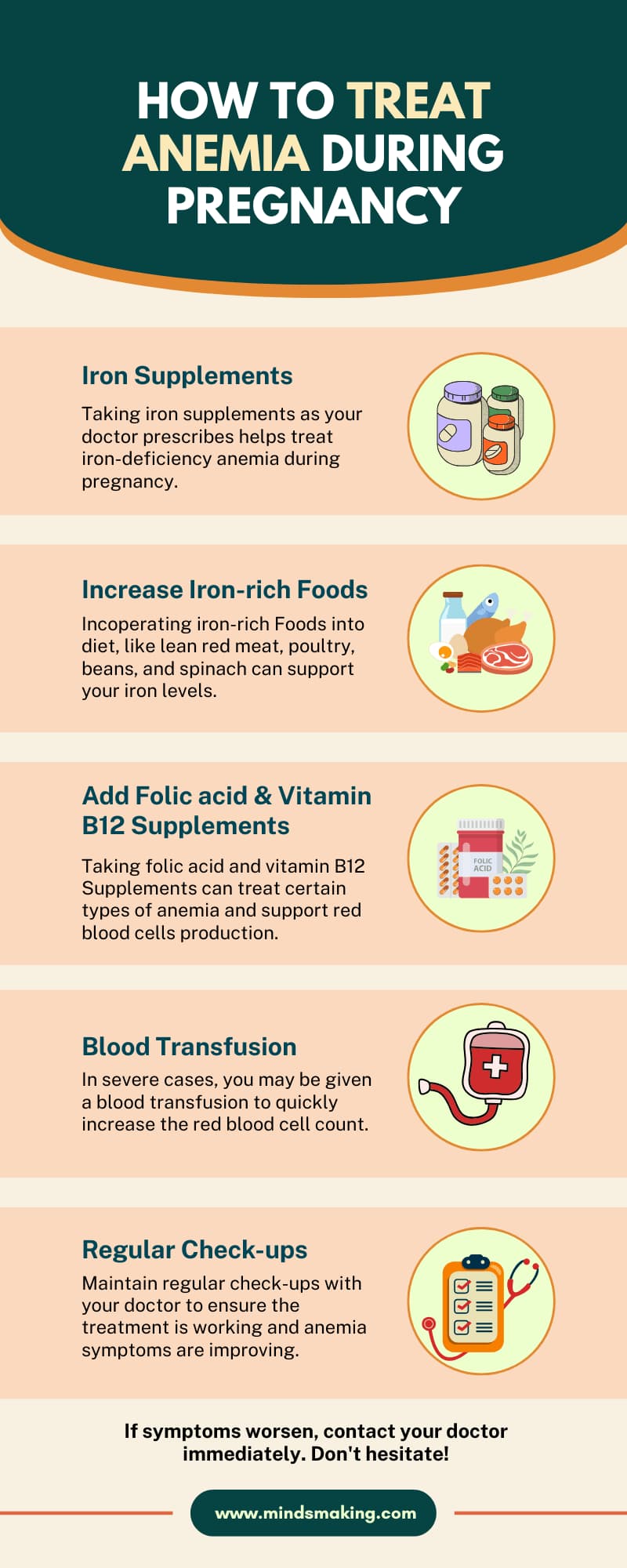
How to Treat Anemia During Pregnancy
Experts say that one of the primary ways to treat iron-deficiency anemia during pregnancy is to use iron supplements and an iron-rich diet. (18)
While a healthy pregnancy diet includes iron-rich foods, it is not enough to reverse anemia on its own once it has developed. This is where the doctors will prescribe iron supplements, and once taken as prescribed, the condition should improve. (17)
The recommended daily intake of elemental iron during pregnancy is 27 mg, but if a woman is anemic, she may need higher doses as directed by her doctor. (11)
The best ways to take iron supplements
- Taking iron supplements on an empty stomach helps your body absorb them better. But they can sometimes make you feel a bit nauseous or cause cramping. If that happens, taking them with a small snack is totally okay to ease the discomfort.
- Vitamin C boosts iron absorption, so taking it with a source of vitamin C, like a little orange juice or a vitamin C tablet, can help your body absorb it better.
- Some foods and drinks can make it harder for the body to absorb iron. It is helpful to avoid dairy, caffeine, soy, spinach, or whole grains for about an hour before and two hours after taking your supplement.
- Calcium supplements or antacid tablets should not be taken at the same time. If you experience nausea, try taking it before going to bed or switch to gummies and liquids. Infusions or injections are available and effective. (18)
The role of folic acid and vitamin B12 in managing anemia
Folic acid and vitamin B12 are important in managing folic acid deficiency anemia and vitamin B12 deficiency anemia during pregnancy. Folic acid supports the formation of red blood cells and helps prevent neural tube defects in the developing baby. (27)
Also, a lack of vitamin B12 can cause similar symptoms and may also lead to neurological complications for both mother and baby if not treated. Taking folic acid and vitamin B12 supplements is necessary when these deficiencies are identified, and they may be given as part of the prenatal vitamin or as additional supplements, depending on the severity. (24), (27)
Best iron-rich foods to maintain iron levels
Eating iron-rich foods can also help keep your iron levels up. Some good foods to include in your pregnancy diet are: (17)
- Lean red meat
- Poultry such as chicken or turkey
- Liver (in small amounts due to the high level of Vitamin A)
- Beans and lentils
- Tofu
- Dark leafy greens like spinach or kale
- Iron-fortified cereals and breads
- Dried fruits like apricots and raisins
mindsmaking
How to Prevent Anemia During Pregnancy
To prevent anemia during pregnancy, focus on a diet rich in iron and folic acid, supplemented with prenatal vitamins. Iron-rich foods. Prenatal vitamins contain iron and folic acid, and your doctor may recommend additional iron supplements if needed. (8) Regular iron supplements during pregnancy, as suggested by ACOG, can help prevent anemia and ensure both mom and baby stay healthy. (16)
- Eat a Balanced, Iron-Rich Diet. Include iron-rich foods like lean red meat, chicken, and fish (animal sources are absorbed more easily), dark green leafy vegetables (like spinach), dried beans, peas, and Iron-fortified cereals. (22)
- To help your body absorb more iron, pair plant-based iron foods or supplements with vitamin C-rich options like orange juice, strawberries, or tomatoes.
- Take prenatal vitamins daily. Prenatal vitamins typically contain iron and folic acid, both crucial for preventing anemia. (22)
- Don’t take iron supplements alongside calcium-fortified juices or dairy products, as calcium interferes with iron absorption.
- Attending regular health check-ups is important for keeping both mother and baby healthy. During these visits, doctors check the blood to see if anemia is present. Iron and folic acid tablets are given to help the body make more red blood cells.
If the anemia is serious and does not improve with tablets, iron through a drip or sometimes a blood transfusion will be given. Regular visits help catch problems early and ensure mother and baby stay safe and strong.(21)
mindsmaking

Frequently Asked Questions
Is anemia common in pregnancy?
Yes, anemia is common during pregnancy, particularly iron-deficiency anemia. It is often due to the increased blood volume and the baby's need for iron, leading to a lower percentage of red blood cells.
Can severe anemia affect my baby?
Yes, severe anemia during pregnancy can negatively affect a baby. It can increase the risk of preterm birth, low birth weight, and potentially lead to a baby developing anemia later in infancy. In some cases, it can also lead to neurodevelopmental issues.
Can anemia cause fatigue during pregnancy?
Yes, it is one of the symptoms of anemia that can be overlooked. It is caused by insufficient red blood cells, which are responsible for carrying oxygen to the tissues in the body. Because of the low delivery of oxygen, symptoms like fatigue, weakness, and shortness of breath can occur.
What foods should I eat to help prevent or treat anemia?
Incorporate iron-rich foods, vitamin C-rich foods, and vitamin B12 into your diet. Iron-rich foods include red meat, poultry, fish, shellfish, beans, lentils, and dark green leafy vegetables. Also, include citrus fruits, berries, and vegetables like tomatoes and peppers. If you are deficient in vitamin B12, include animal products like meat, poultry, and fish.
What if anemia is not treated during pregnancy?
Anemia, if not treated during pregnancy, can lead to serious complications, including premature birth, low birth weight, and increased risk of complications during delivery. In some cases, untreated anemia can even lead to fetal death or maternal mortality.
How does anemia during pregnancy affect labor and delivery?
Anemia during pregnancy can increase the risk of complications during labor and delivery, including premature birth, low birth weight, and postpartum hemorrhage. It can also make it harder for the mother to fight infections and increase the risk of needing a blood transfusion. (14)
How long does it take to recover from anemia during pregnancy?
Some studies suggest that anemia recovery can take five to ten months, while others indicate it may require up to 180 days for optimal recovery.
Is anemia more common in certain trimesters of pregnancy?
Yes, anemia is generally more common in the third trimester of pregnancy, although it can occur in any trimester. Many women lack the sufficient amount of iron needed for the second and third trimesters. When your body needs more iron than it has available, you can become anemic.
Can anemia during pregnancy lead to postpartum anemia?
Yes, anemia during pregnancy can increase the likelihood of developing postpartum anemia. Low iron levels during pregnancy can be carried over into the postpartum period, and blood loss during delivery can also deplete iron stores, leading to anemia.
Was this article helpful?
How many stars are you giving this article?
Leave a comment
Your email address will not be published.









































