Hyperemesis Gravidarum
fluky fluky

Written by Mindsmaking Medical Writer
Fact Checked by Mindsmaking Professionals
2nd, June, 2025
Not all pregnancy nausea is just morning sickness. Hyperemesis gravidarum is a severe condition that causes persistent vomiting, dehydration, and weight loss, sometimes lasting the entire pregnancy.
In the early stages of pregnancy, it’s normal to experience some nausea and vomiting. However, when it becomes constant, intense, and makes it difficult to eat, drink, or carry out daily activities, it may be a more serious condition known as hyperemesis gravidarum.
Hyperemesis gravidarum is more than just your normal morning sickness. It is much more severe and can lead to dehydration, weight loss, and ketosis, making you feel drained.
The feeling of being unable to keep anything down and function like you normally do can be depressing and frustrating. But you do not have to go through it without help. With the right support, such as medication or IV fluids, your symptoms can be managed, helping you feel more like yourself again and easing the challenges of this phase.
Key Takeaways
Hyperemesis Gravidarum (HG) is a severe and persistent form of nausea and vomiting during pregnancy that is far beyond the typical morning sickness. It occurs in approximately 0.3% to 2% of pregnancies in the United States.
According to the National Institutes of Health, the cause of hyperemesis gravidarum is not fully understood but is thought to involve a combination of factors, including hormones, genetics, and changes in the gastrointestinal system.
Symptoms of hyperemesis gravidarum include: persistent nausea and vomiting, inability to keep food or liquids down, weight loss, fatigue, severe headaches, and feeling of isolation.
An assessment, physical examination, and laboratory tests would be carried out before hyperemesis gravidarum can be diagnosed.
In the treatment and management of hyperemesis gravidarum, medications such as metoclopramide, IV fluids, dietary adjustments, eating tips, and hydration strategies are often required.
What is Hyperemesis Gravidarum?
Hyperemesis Gravidarum (HG) is a severe and persistent form of nausea and vomiting during pregnancy that is far beyond the typical morning sickness. It can lead to dehydration, significant weight loss, which is more than 5% of your pre-pregnancy weight gone, electrolyte imbalances, and in serious cases, hospitalization. (8)
Most pregnant women, up to 90%, feel some level of nausea, and about 27% to 30% feel only nausea without actually vomiting. However, hyperemesis gravidarum, which is a much more severe form of nausea and vomiting, is rare. It affects about 0.3% to 3% of pregnancies in the U.S. and is seen more often in Western countries. (8)
Hyperemesis gravidarum occurs early, from 4 to 6 weeks into pregnancy, with the symptoms at their peak between 9 and 13 weeks. (1)
Unlike morning sickness, which eases up by the end of the first trimester (12 to 14 weeks), hyperemesis gravidarum can last much longer. Sometimes into the second trimester or even throughout your entire pregnancy. (1)
Morning sickness can sometimes be managed with dietary changes and home remedies. However, hyperemesis gravidarum usually requires medical intervention, such as IV fluids, anti-nausea medications, and, in some cases, hospitalization.
For some pregnant women, the worst of it eases up by mid-pregnancy, but for others, approximately 10%, the nausea and vomiting can continue until delivery. (8)
Living with HG can be physically and emotionally draining, and it requires ongoing support from healthcare providers and family to get through each day.
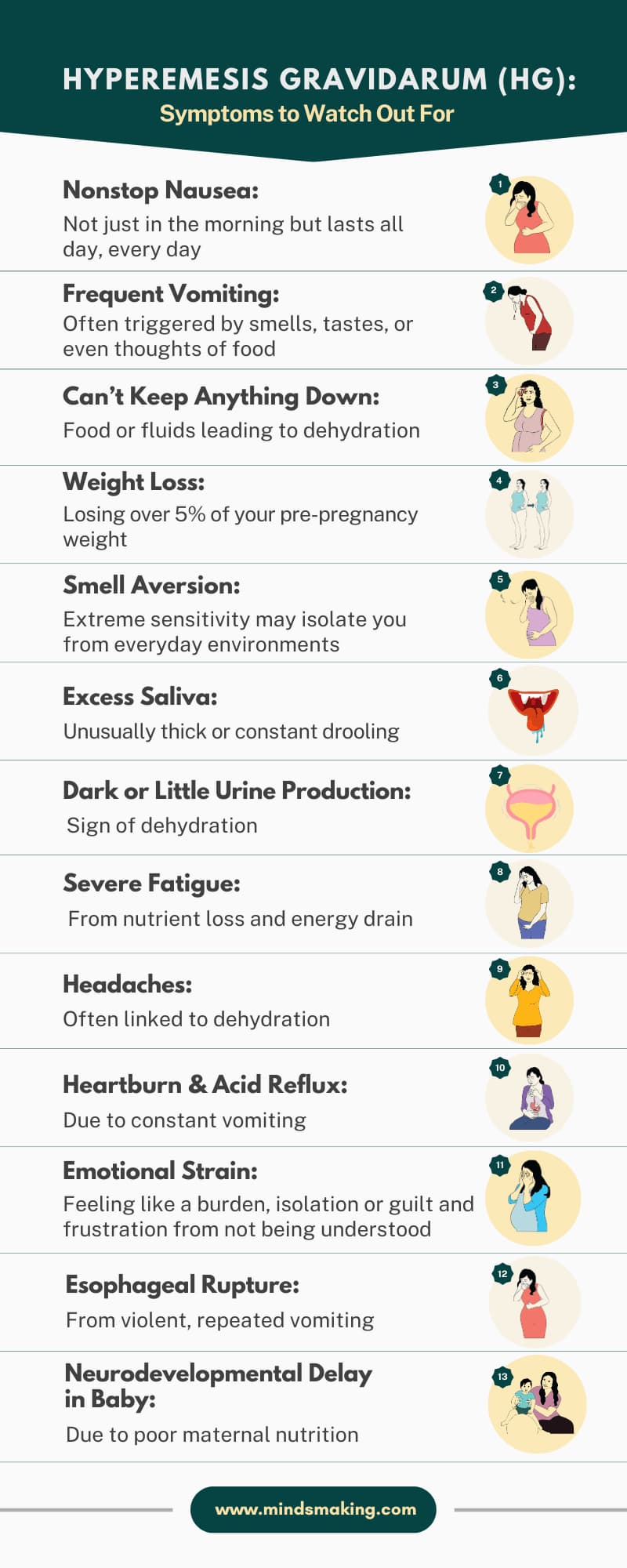
Symptoms Of Hyperemesis Gravidarum To Watch Out For?
At first, hyperemesis gravidarum can resemble regular morning sickness, making it easy to dismiss. The symptoms to watch out for in the early stages include:
- Persistent nausea and vomiting that does not subside after the first trimester.
- Unable to keep food or fluids down, leading to dehydration.
- Weight loss of more than 5% of your pre-pregnancy body weight.
- Frequent vomiting may be triggered by smells, tastes, or even the thought of food.
- Dark urine or minimal urine production, which could indicate dehydration.
- Excessive salivation
As hyperemesis gravidarum progresses, it can lead to other physical and emotional symptoms, including:
- Fatigue due to the constant vomiting and lack of nutrition.
- Severe headaches due to dehydration.
- Heartburn due to frequent vomiting, acid reflux can become an issue.
- Feelings of being a burden, isolation, frustration, and guilt. This is especially true if you can't take care of your day-to-day responsibilities, and people don't understand what you're going through. (1)
Ysis Lorenna, a mother of 2, shares her experience with hyperemesis gravidarum. She explains that she was five weeks into her third pregnancy when she started experiencing nausea and vomiting.
At first, she thought it was the usual morning sickness she had experienced during her first and second pregnancies, but not until the nausea became relentless (24/7), which was causing her not to want to eat anything, and she fell ill multiple times a day.
She had a smell aversion to everything, causing her to stay in her bedroom most of the time. She was so weak and dehydrated that about seven weeks into her pregnancy, she had lost 14 pounds of her pre-pregnancy weight.
mindsmaking
What Causes Severe Nausea and Who Is Most at Risk?
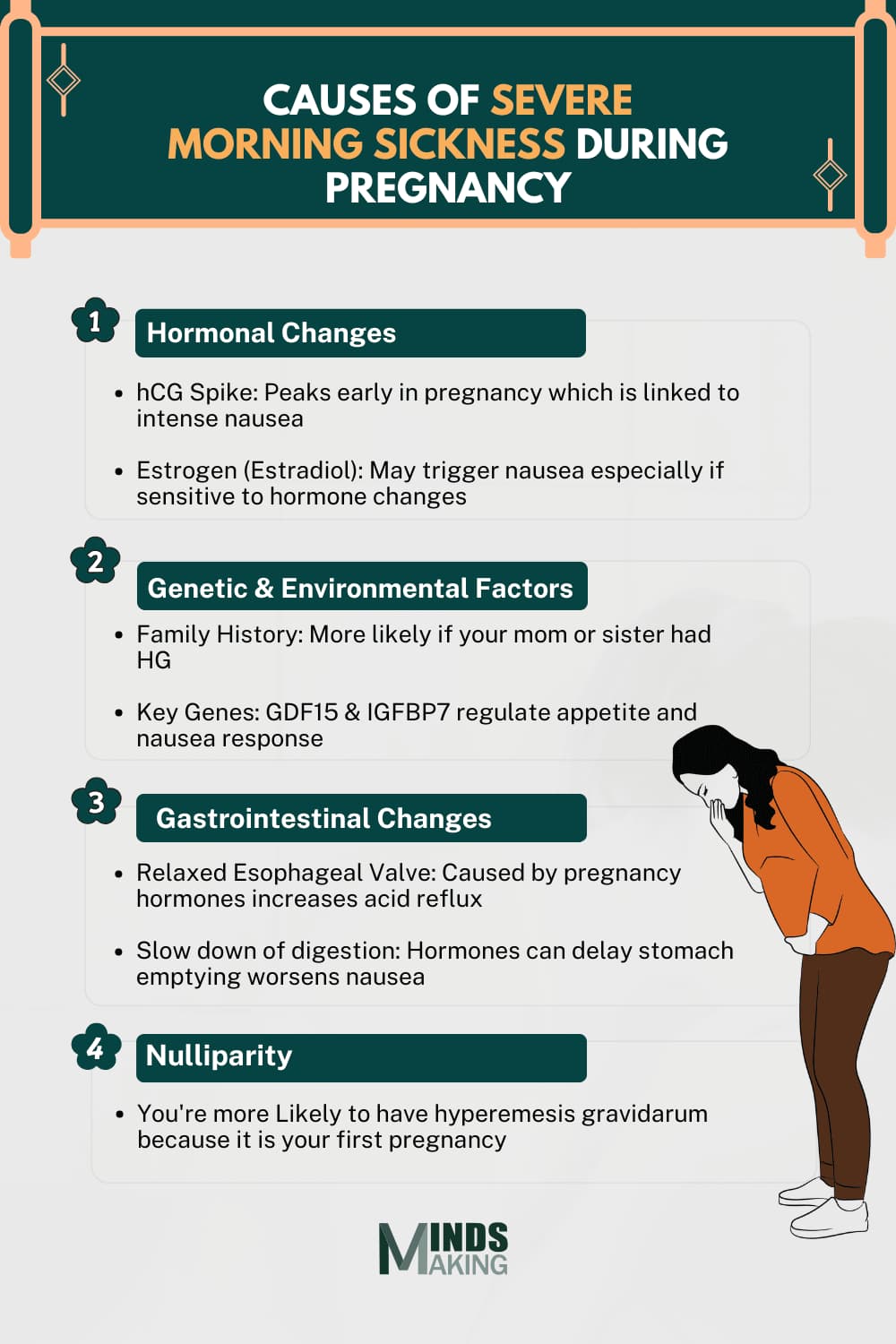
According to the National Institutes of Health, the cause of hyperemesis gravidarum is not fully understood. Still, it is thought to be due to a combination of factors, including hormones, genetics, and changes in the gastrointestinal system. (8)
Hormonal Changes
Hormonal fluctuations, especially in the first trimester, are among the most widely studied contributors to hyperemesis gravidarum. One key hormone involved is human chorionic gonadotropin (hCG).
hCG levels naturally rise in early pregnancy and are at their peak around the time hyperemesis gravidarum symptoms usually appear. Some studies suggest that higher hCG levels are linked to more intense nausea, though research is still ongoing. (12)
Estrogen, particularly a type called estradiol, rises early in pregnancy and may play a role in nausea. This is supported by the fact that some people experience nausea when taking medications that contain estrogen.
Genetics and Environmental Factors
If severe nausea runs in your family, you might be more likely to experience it yourself. Researchers have found that certain genes, such as GDF15 and IGFBP7, may be linked to HG. These genes are linked to how the body responds to pregnancy and regulate factors such as appetite and nausea. (13)
Changes Gastrointestinal System
Pregnancy hormones like estrogen and progesterone can relax the lower esophageal sphincter, the muscle that keeps stomach acid where it belongs. This increases the chances of acid reflux, which is common in pregnancy and can make nausea even worse.
Some studies have looked at the connection between gastroesophageal reflux (GERD) and vomiting in pregnancy, but the findings are mixed. Still, changes in how your digestive system works can add to the discomfort. (14)
Other factors that increase the likelihood of hyperemesis gravidarum include (9):
- Multiple pregnancies (twins, triplets)
- Family history of hyperemesis gravidarum
- A history of hyperemesis gravidarum in a previous pregnancy
- Being of a young maternal age
- History of abortion
- Pregnant with a girl
- Nulliparity (first pregnancy)
- Helicobacter pylori infection (a bacterial infection that can cause gastritis and peptic ulcers)
Read This Next
No posts available
mindsmaking
The Dangers of Untreated Hyperemesis Gravidarum
As hyperemesis gravidarum progresses, it can lead to other complications and even death if left untreated. (4)
One such complication is electrolyte imbalance. Dehydration can disrupt the balance of electrolytes in your body, leading to complications.
Another complication is liver damage. Because of the persistent nausea, vomiting, and dehydration, the liver can get damaged, which potentially leads to jaundice and liver failure.
Also, Wernicke encephalopathy and esophageal Rupture can develop. Wernicke encephalopathy can cause imbalance, confusion, and dizziness. The esophageal rupture is caused by constant and severe vomiting.
Other complications include: Placental abruption, preeclampsia, and neurodevelopmental delay of the fetus due to malnutrition.
When to Call Your Doctor About Nausea and Vomiting During Pregnancy
Not sure if your nausea is normal or something more serious? Morning sickness is common, but if it starts interfering with your daily life, it could be a sign of something more serious, like hyperemesis gravidarum. Don’t ignore your symptoms; knowing when to call your doctor can help you feel better and protect your baby’s health.
Reach out to your doctor if you experience any of the following:
- You can’t keep food or fluids down for more than 24 hours
- You’re losing weight instead of gaining during pregnancy.
- You feel extremely tired, dizzy, or faint.
- Your urine is very dark, or you’re urinating less often.
- You have stomach pain, fever, or vomiting blood.
- You’re unable to function or perform daily tasks.
- Your symptoms are getting worse instead of better
Getting medical help early can make a big difference. Don’t wait, your body and baby need care.
How Doctors Diagnose Hyperemesis Gravidarum
To diagnose hyperemesis gravidarum, an assessment, physical examination, and laboratory tests would be carried out.
The process for the diagnosis first starts with:
An assessment of your symptoms: Severe nausea and vomiting that leads to dehydration (signs of this might show up in a urine test as ketones or electrolyte imbalance), weight loss of about 5% of your pre-pregnancy weight without any other cause for the vomiting, like an infection or gastrointestinal condition. (8)
A Physical Examination: Doctors will check vital signs, such as blood pressure and heart rate, to assess your overall health and rule out other conditions. Next is an abdominal exam to assess for any unusual tenderness or vaginal bleeding. Lastly, a thyroid evaluation to assess your thyroid function, as thyroid disorders can sometimes mimic the symptoms of hyperemesis.
Laboratory Tests: These include blood and urine tests. Blood tests assess electrolyte levels, kidney function, and liver function to rule out other conditions and determine the severity of dehydration. Urinalysis will check for the presence of ketones, which may indicate how dehydrated you are.
Obstetrical Ultrasound: An ultrasound would be carried out to rule out multiple pregnancies, ectopic pregnancy, and check for any gestational trophoblastic disease which is depending on your history and previous obstetrical evaluations.
Alternative Diagnosis: A radiographic study may be performed to rule out other diseases. Magnetic resonance imaging (MRI) will also be used to assess alternative diagnoses, such as appendicitis.
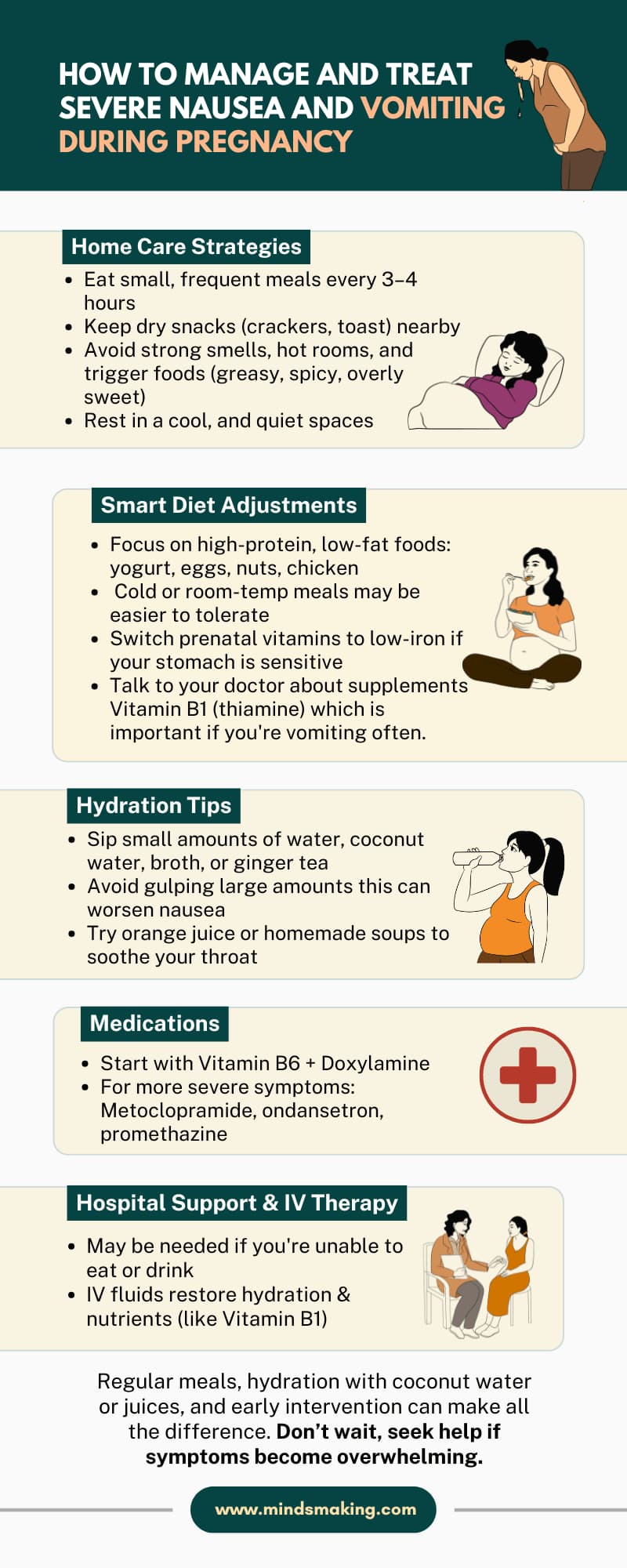
How to Manage and Treat Severe Nausea and Vomiting During Pregnancy
Dr. Muthineni Rajini shares her expert insight on managing hyperemesis gravidarum, highlighting treatments like anti-nausea medications, IV fluids, and simple home strategies, such as eating small, frequent meals every 3 to 4 hours, to help ease symptoms and support recovery.
Here’s a closer look at how each of these approaches can help:
Home Care Strategies
Sometimes, small lifestyle changes can go a long way in easing your symptoms. Try eating small, frequent meals throughout the day. This keeps your stomach from getting too empty, often worsening your nausea.
Keep snacks like dry crackers or toast nearby, especially in the morning. Avoid strong smells, hot rooms, and foods that are too spicy, greasy, or sweet. Many people find relief by resting in a cool, quiet space or using motion-sickness bands on their wrists. (15)
Diet Adjustments and Eating Tips
When your nausea reduces to the point where you feel like you can’t eat, focus on high-protein, low-fat foods that are easy to digest. Eat nuts, yogurt, eggs, or small portions of chicken or beans. Cold or room-temperature foods may also be easier on your stomach.
If you're taking prenatal vitamins, consider switching to one with lower iron content, as too much iron can sometimes irritate your stomach.
Vitamin B1 (thiamine) is especially important if you experience frequent vomiting. Before taking it, speak with your doctor. (10)
Hydration Strategies
Staying hydrated can be challenging, but it’s crucial. Instead of drinking large amounts at once, which might trigger nausea, try sipping small amounts of fluids throughout the day. Clear liquids like water, broth, ginger tea, or electrolyte drinks are gentle on the stomach and can help you stay hydrated without worsening your symptoms.
Look out for signs of dehydration, such as dark urine, dizziness, dry mouth, or a rapid heartbeat, and contact your healthcare provider if you notice any of these symptoms. (11)
Medications
If changes to your diet and routine aren’t enough, safe medications can help. Many doctors start with a combination of vitamin B6 (pyridoxine) and doxylamine, which is also found in some over-the-counter sleep aids.
For more severe symptoms, your doctor may prescribe medications such as metoclopramide, ondansetron, or promethazine. Don’t hesitate to ask about the safety of these medications and any potential side effects; your comfort and peace of mind matter (3).
Hospitalization and IV therapy
If you’re unable to eat, feel very weak, or start getting dehydrated, your doctor may recommend a short stay in the hospital. There, you’ll receive IV fluids to rehydrate and restore essential nutrients, such as thiamine (vitamin B1).
Some hospitals also offer outpatient IV therapy, allowing you to get the support you need without being fully admitted (7).
mindsmaking
Frequently Asked Questions
How is hyperemesis gravidarum different from morning sickness?
Hyperemesis gravidarum is different from morning sickness because it is characterized by persistent and severe nausea and vomiting that can lead to dehydration, electrolyte imbalance, and weight loss, while morning sickness is a milder form of it.
What are the first signs of hyperemesis gravidarum?
Persistent nausea and vomiting that does not subside after the first trimester, inability to keep food or fluids down, weight loss of more than 5% of your pre-pregnancy body weight, dark urine or very little urine production, and excessive salivation.
Can hyperemesis gravidarum harm my baby?
Yes. Severe vomiting during pregnancy can potentially harm your baby if not treated in time. It can lead to low birth weight, preterm birth, and other complications.
Are there natural remedies that work for HG?
Yes, some natural remedies can help manage the symptoms of Hyperemesis Gravidarum (HG), but sometimes medical treatment is necessary for severe cases. Dietary changes like eating small, frequent, bland meals, staying hydrated, and avoiding triggers can be helpful.
When should I go to the hospital for hyperemesis gravidarum?
If you can't tolerate fluids for over 12 hours, or if you experience severe abdominal pain or blood in your vomit. Also, if you develop signs of dehydration like dark urine, decreased urination, dizziness, or fainting, and you notice you are losing weight.
Will HG affect all my pregnancies?
If you've had hyperemesis gravidarum (HG) in your previous pregnancy, the likelihood of it recurring in your future pregnancies is high. Recent research by the HER Foundation finds that over half of women (about 2/3rds) will have HG in every pregnancy.
How can I get enough nutrition if I can’t eat?
If your case is severe to the point that you can't even eat anything, your doctor would recommend you come to the hospital to receive IV fluids and rehydrate yourself, and also nutrients like thiamine.
How long does hyperemesis gravidarum last?
It depends. Hyperemesis gravidarum occurs early, from 4 to 6 weeks into pregnancy, with the symptoms at their peak between 9 and 13 weeks. (1) For some pregnant women, the worst of it eases up by mid-pregnancy, but for others, approximately 10%, the nausea and vomiting can continue until delivery.
Can hyperemesis gravidarum be prevented?
Hyperemesis gravidarum cannot be fully prevented, but with certain strategies, you can reduce the severity of symptoms if the symptoms develop. Preparing for pregnancy and seeking early treatment can be helpful.
Was this article helpful?
How many stars are you giving this article?
Leave a comment
Your email address will not be published.









































