Menu

Congratulations on reaching the second trimester! This is an exciting time as your baby bump becomes more noticeable. During weeks 14 to 27, you can expect various changes. Your body might undergo shifts like increased energy, reduced morning sickness, and the joy of feeling your baby’s first kicks.
It’s also an ideal period for sharing your pregnancy news with others. In this article, we’ll discuss your baby’s development, concerns, and important things to remember during this part of your pregnancy journey.
The second trimester of pregnancy is often the most enjoyable because troublesome early symptoms tend to fade, bringing a sense of normalcy. While some may start feeling more like themselves, not everyone experiences this relief.
The second trimester can still bring new or recurring symptoms and body changes.

During pregnancy, your belly grows as your uterus expands to accommodate the growing baby. Simultaneously, your breasts will gradually increase in size. It’s important to provide proper support, and wearing a supportive bra with wide straps or a sports bra can be essential. This helps minimize discomfort and provides the necessary support for the changes your body is undergoing.

In the second trimester, you might feel some aches or cramps in your lower belly. This happens because your growing uterus puts pressure on nearby muscles and ligaments. The round ligament muscle can cramp as it stretches, causing a dull ache or occasional sharp pains.
These cramps are usually normal and can be triggered by things like constipation, gas, or sexual activity. Try a warm bath, relaxation exercises, changing your position, or placing a hot water bottle wrapped in a towel on your lower belly to ease the discomfort.

Braxton Hicks contractions are mild, irregular contractions that you may feel as a slight tightness in your abdomen. They often occur more frequently in the afternoon or evening, particularly after physical activity or sex.
While these contractions are usually harmless, reaching out to your healthcare provider is crucial if they become regular and consistently strengthen. This could indicate preterm labour and early detection is essential for proper medical attention and care.
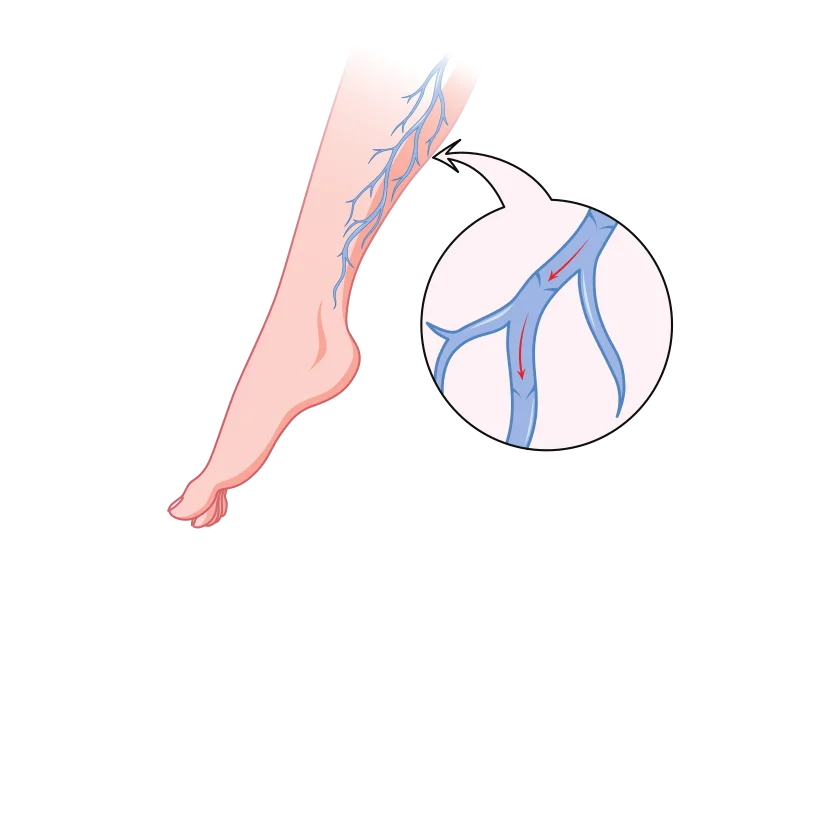
Increased blood circulation during pregnancy, meant to support your growing baby, can lead to the appearance of tiny red veins known as spider veins. These usually fade after childbirth. Additionally, pressure on your legs from your expanding baby may slow blood flow, resulting in swollen and blue or purple veins called varicose.
While avoiding varicose veins may be challenging, you can prevent worsening by staying active, propping up your legs when sitting for extended periods, and wearing a support hose for added support. Varicose veins typically improve within three months after delivery.
As your pregnancy advances, the extra weight you’ve gained may cause backache and soreness. To ease this, sit up straight in chairs with good back support and sleep on your side with a pillow between your legs.
Avoid lifting heavy things and wear comfortable shoes. If your back is sore, ask your partner for a gentle massage or treat yourself to a pregnancy massage for relief.

During pregnancy, hormonal changes can cause skin alterations. You might see brown patches on your face (melasma) or a dark line down your abdomen (linea nigra). These changes are common and usually fade after giving birth.
Protect your skin from the sun with sunscreen when outdoors, as sun exposure can worsen these issues.
You may also notice stretch marks, which can appear in various colours on your abdomen, breasts, buttocks, or thighs. While you can’t prevent stretch marks, they often fade over time.
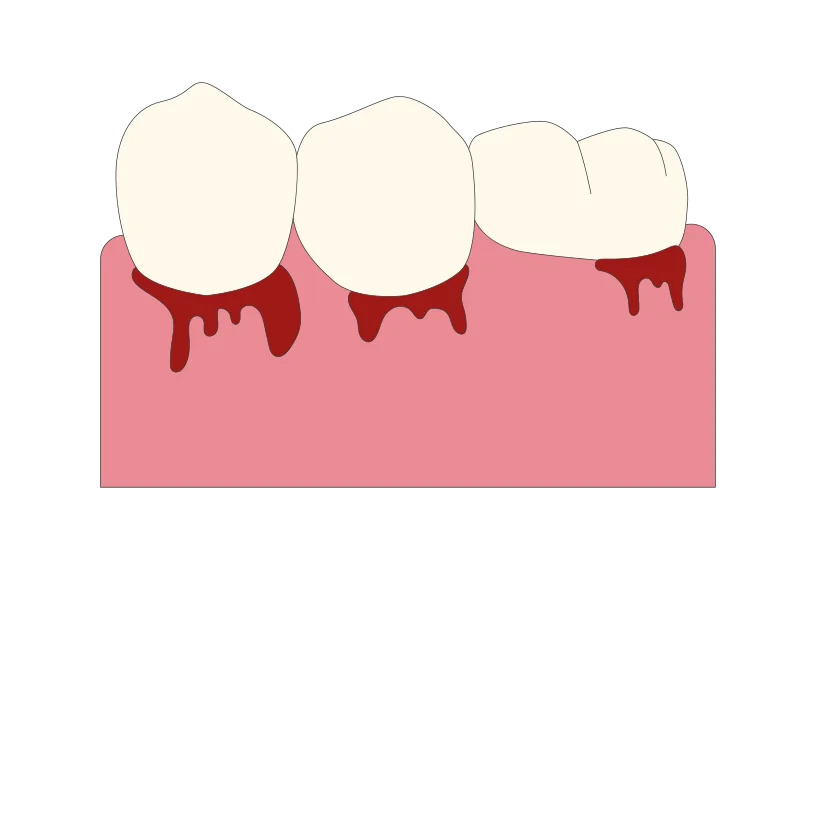
During pregnancy, about half of women might notice that their gums become swollen, tender, and bleed more easily. This happens because hormonal changes increase blood flow to the gums. While this usually goes back to normal after giving birth, it’s crucial to maintain good oral hygiene.
Use a softer toothbrush, be gentle when flossing, and don’t skip regular dental care. Studies suggest a connection between gum disease during pregnancy and a higher risk of premature labour and delivering a low-birth-weight baby, underscoring the importance of taking care of your oral health while expecting.

During pregnancy, hormonal changes might cause your nose to get stuffy and bleed more easily. This happens because the tissues inside your nose swell. If you’re congested, check with your doctor before using decongestants. Instead, try saline drops or natural methods to ease congestion.
Using a humidifier can also help. If you get a nosebleed, keep your head straight (don’t tilt it back) and press on the nostril for a few minutes until the bleeding stops.
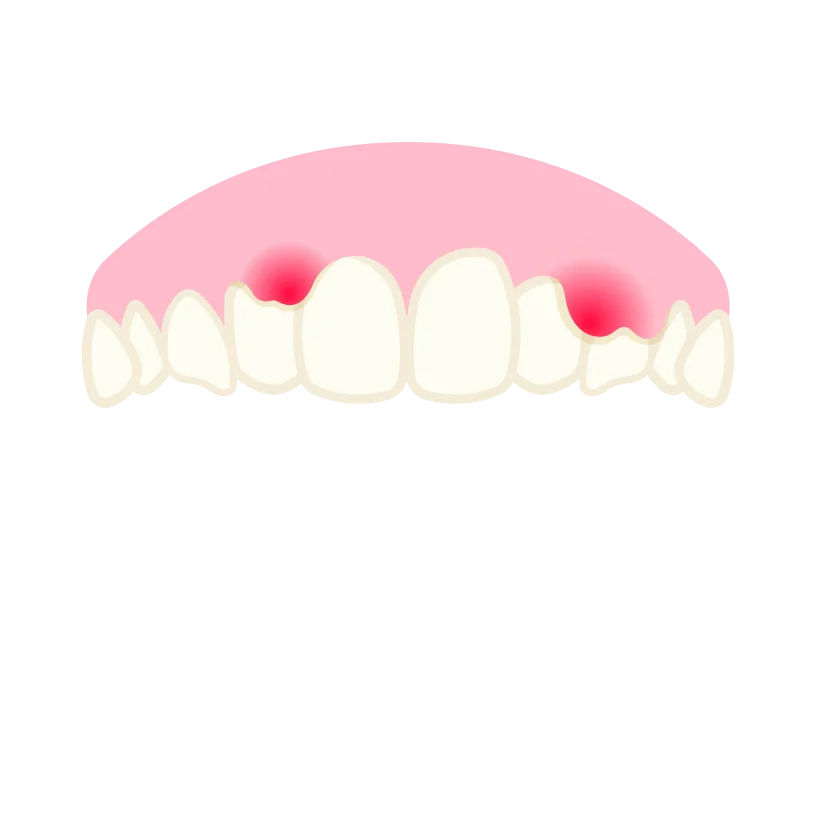
Pregnancy can make your gums more sensitive, leading to minor bleeding while flossing and brushing. To reduce irritation, consider rinsing with salt water and using a softer toothbrush. Additionally, frequent vomiting, often associated with morning sickness, can affect your tooth enamel and increase the risk of cavities.
Maintaining regular dental care during pregnancy is crucial, addressing gum sensitivity and taking preventive measures to protect your teeth, such as using fluoride toothpaste and consulting your dentist for advice on maintaining oral health throughout this period.
Urinary tract infections (UTIs) are common during pregnancy. Suppose you feel a strong, urgent need to urinate, experience sharp pain, notice cloudy or strong-smelling urine, or have a fever or backache. In that case, it’s important to contact your healthcare provider. If untreated, UTIs can become severe, potentially leading to a kidney infection.
Seeking prompt medical attention is crucial to address and prevent complications associated with urinary tract infections during pregnancy.
As morning sickness subsides by the end of the first trimester, your appetite typically returns and might even increase. While food becomes more appealing, being mindful of your eating habits is essential.
During the second trimester, you only need around 300 to 500 calories daily, and your weight gain should be approximately 1/2 to 1 pound per week. Balancing your nutrition is important for your well-being and your baby’s healthy development during pregnancy.
During early pregnancy, it’s common to notice a thin, milky white vaginal discharge known as leukorrhea. While wearing a panty liner for comfort is fine, avoid using tampons as they can introduce germs into the vagina.
However, if the discharge becomes foul-smelling, green or yellow, contains blood, or if you experience a significant increase in clear discharge, it’s essential to contact your doctor for guidance, as these could be indicators of potential issues that need attention.
Leg cramps are common as pregnancy progresses, especially at night. To prevent them, consider stretching your calf muscles before bedtime, staying physically active, and ensuring you stay well-hydrated. Opt for comfortable and supportive shoes that prioritize utility.

Quickening refers to the first subtle movements you feel in your abdomen, typically around the midpoint of your pregnancy, usually around 20 weeks. There’s no need to worry if you haven’t felt these movements yet.
Some women don’t experience quickening until the sixth month of pregnancy. It’s a unique and individual experience, so the timing can vary for different women.

Dizziness during the second trimester can result from your expanding uterus pressing against blood vessels or blood sugar and hormone fluctuations. To manage this, avoid standing for extended periods, rise slowly from sitting or lying positions, maintain regular meals and snacks, and stay well-hydrated.
Choose loose clothing and refrain from hot showers or baths. Also, avoid lying flat on your back for the rest of your pregnancy. If dizziness is accompanied by fainting, vaginal bleeding, or abdominal pain, it’s crucial to contact your doctor for guidance and evaluation.
Heartburn and constipation during pregnancy are often attributed to increased hormone progesterone levels. This hormone relaxes specific muscles, including the lower oesophagal muscle ring that usually keeps food and acids in your stomach and the muscles responsible for moving digested food through your intestines.
To alleviate heartburn, consider having more frequent, smaller meals and avoiding greasy, spicy, and acidic foods. Increase your fibre intake for constipation and stay well-hydrated to facilitate smoother digestion. Engaging in physical activity can also be beneficial in promoting regular bowel.
Hemorrhoids are like swollen veins around the bottom; they can become itchy and uncomfortable during pregnancy. This happens because of increased blood flow and pressure from the growing uterus.
Try sitting in a warm tub or sitz bath to ease the discomfort. You can also ask your doctor about using over-the-counter haemorrhoid ointments for relief.

Pregnancy hormones can lead to increased hair growth, making the hair on your head thicker. However, you might also notice hair in new places like your face, arms, or back. While shaving and tweezing are generally considered safe options during pregnancy.
It is advised to stay away from laser hair removal, electrolysis, waxing, or depilatories.
Headaches are common during pregnancy. Relaxation techniques like deep breathing can help. Avoid aspirin and ibuprofen, but if the headaches bother you, check with your doctor if it’s okay to take acetaminophen.
Always consult your healthcare provider before taking any medication during pregnancy.

During pregnancy, your belly grows as your uterus expands to accommodate the growing baby. Simultaneously, your breasts will gradually increase in size. It’s important to provide proper support, and wearing a supportive bra with wide straps or a sports bra can be essential. This helps minimize discomfort and provides the necessary support for the changes your body is undergoing.

In the second trimester, you might feel some aches or cramps in your lower belly. This happens because your growing uterus puts pressure on nearby muscles and ligaments. The round ligament muscle can cramp as it stretches, causing a dull ache or occasional sharp pains.
These cramps are usually normal and can be triggered by things like constipation, gas, or sexual activity. Try a warm bath, relaxation exercises, changing your position, or placing a hot water bottle wrapped in a towel on your lower belly to ease the discomfort.

Braxton Hicks contractions are mild, irregular contractions that you may feel as a slight tightness in your abdomen. They often occur more frequently in the afternoon or evening, particularly after physical activity or sex.
While these contractions are usually harmless, reaching out to your healthcare provider is crucial if they become regular and consistently strengthen. This could indicate preterm labour and early detection is essential for proper medical attention and care.
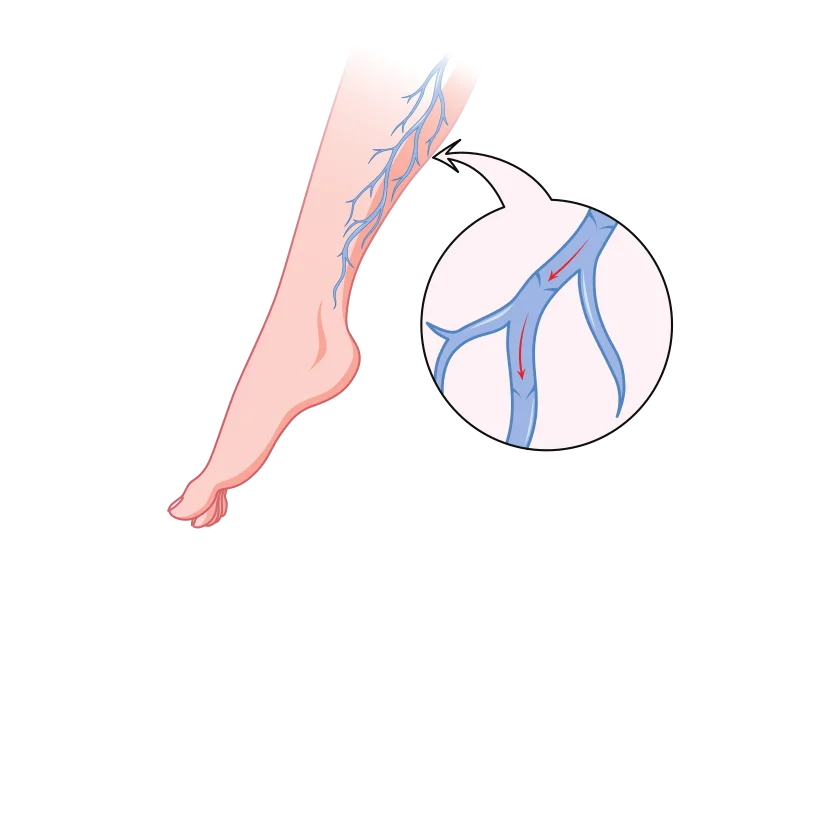
Increased blood circulation during pregnancy, meant to support your growing baby, can lead to the appearance of tiny red veins known as spider veins. These usually fade after childbirth. Additionally, pressure on your legs from your expanding baby may slow blood flow, resulting in swollen and blue or purple veins called varicose.
While avoiding varicose veins may be challenging, you can prevent worsening by staying active, propping up your legs when sitting for extended periods, and wearing a support hose for added support. Varicose veins typically improve within three months after delivery.
As your pregnancy advances, the extra weight you’ve gained may cause backache and soreness. To ease this, sit up straight in chairs with good back support and sleep on your side with a pillow between your legs.
Avoid lifting heavy things and wear comfortable shoes. If your back is sore, ask your partner for a gentle massage or treat yourself to a pregnancy massage for relief.

During pregnancy, hormonal changes can cause skin alterations. You might see brown patches on your face (melasma) or a dark line down your abdomen (linea nigra). These changes are common and usually fade after giving birth.
Protect your skin from the sun with sunscreen when outdoors, as sun exposure can worsen these issues.
You may also notice stretch marks, which can appear in various colours on your abdomen, breasts, buttocks, or thighs. While you can’t prevent stretch marks, they often fade over time.
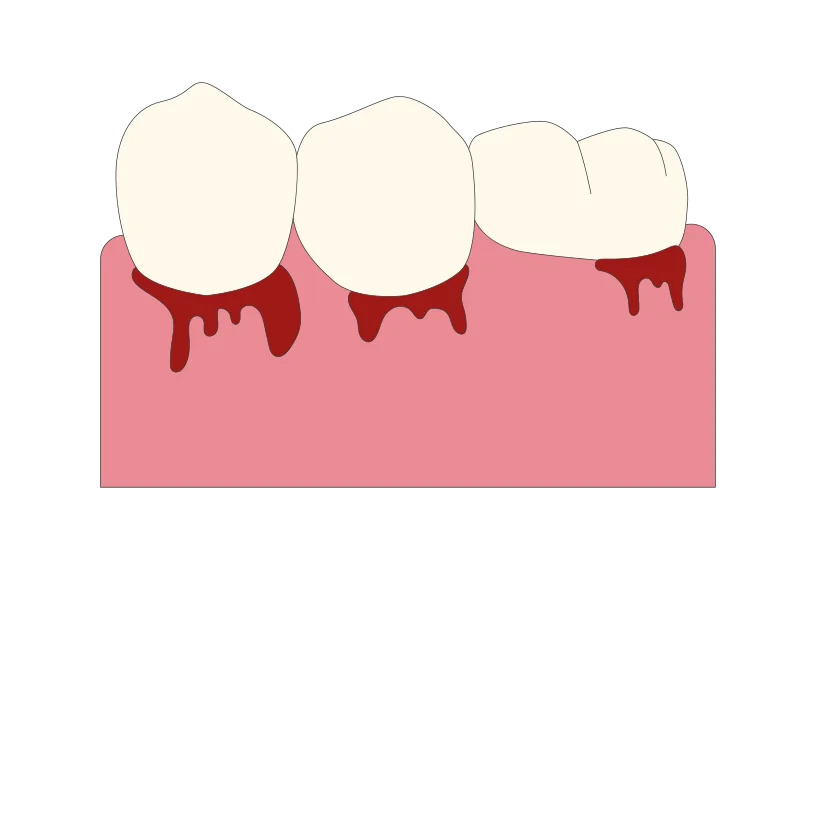
During pregnancy, about half of women might notice that their gums become swollen, tender, and bleed more easily. This happens because hormonal changes increase blood flow to the gums. While this usually goes back to normal after giving birth, it’s crucial to maintain good oral hygiene.
Use a softer toothbrush, be gentle when flossing, and don’t skip regular dental care. Studies suggest a connection between gum disease during pregnancy and a higher risk of premature labour and delivering a low-birth-weight baby, underscoring the importance of taking care of your oral health while expecting.

During pregnancy, hormonal changes might cause your nose to get stuffy and bleed more easily. This happens because the tissues inside your nose swell. If you’re congested, check with your doctor before using decongestants. Instead, try saline drops or natural methods to ease congestion.
Using a humidifier can also help. If you get a nosebleed, keep your head straight (don’t tilt it back) and press on the nostril for a few minutes until the bleeding stops.
Pregnancy can make your gums more sensitive, leading to minor bleeding while flossing and brushing. To reduce irritation, consider rinsing with salt water and using a softer toothbrush. Additionally, frequent vomiting, often associated with morning sickness, can affect your tooth enamel and increase the risk of cavities.
Maintaining regular dental care during pregnancy is crucial, addressing gum sensitivity and taking preventive measures to protect your teeth, such as using fluoride toothpaste and consulting your dentist for advice on maintaining oral health throughout this period.
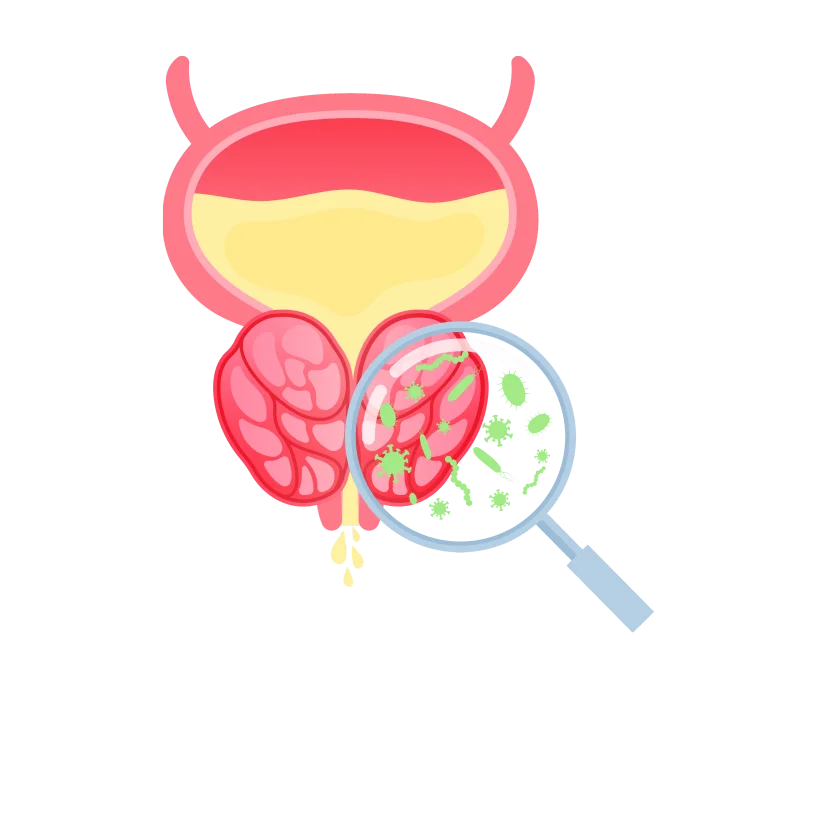
Urinary tract infections (UTIs) are common during pregnancy. Suppose you feel a strong, urgent need to urinate, experience sharp pain, notice cloudy or strong-smelling urine, or have a fever or backache. In that case, it’s important to contact your healthcare provider. If untreated, UTIs can become severe, potentially leading to a kidney infection.
Seeking prompt medical attention is crucial to address and prevent complications associated with urinary tract infections during pregnancy.
As morning sickness subsides by the end of the first trimester, your appetite typically returns and might even increase. While food becomes more appealing, being mindful of your eating habits is essential.
During the second trimester, you only need around 300 to 500 calories daily, and your weight gain should be approximately 1/2 to 1 pound per week. Balancing your nutrition is important for your well-being and your baby’s healthy development during pregnancy.
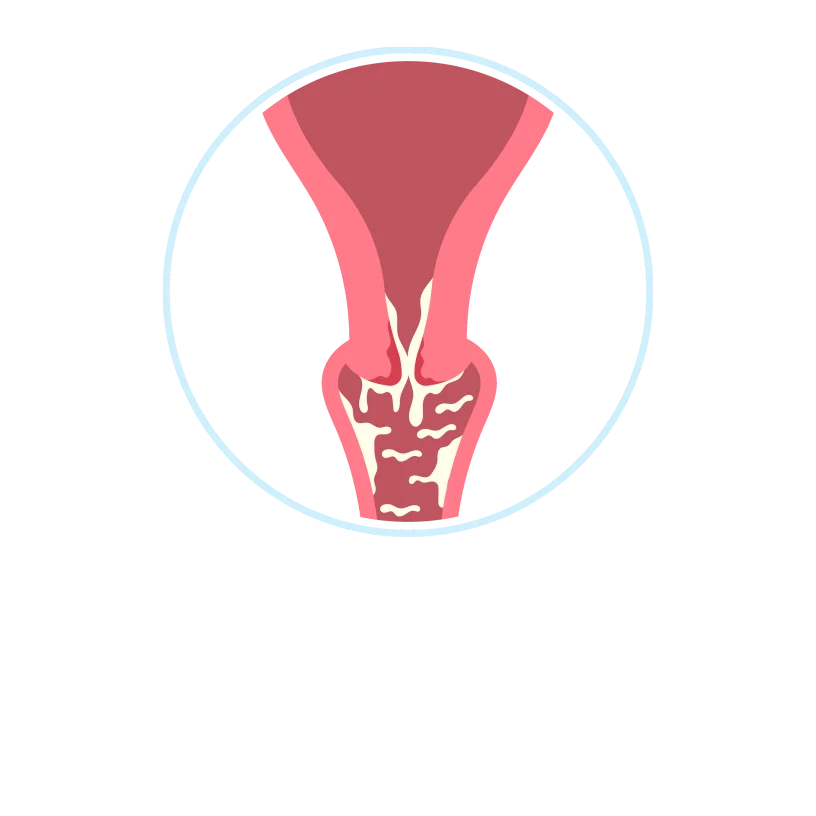
During early pregnancy, it’s common to notice a thin, milky white vaginal discharge known as leukorrhea. While wearing a panty liner for comfort is fine, avoid using tampons as they can introduce germs into the vagina.
However, if the discharge becomes foul-smelling, green or yellow, contains blood, or if you experience a significant increase in clear discharge, it’s essential to contact your doctor for guidance, as these could be indicators of potential issues that need attention.
Leg cramps are common as pregnancy progresses, especially at night. To prevent them, consider stretching your calf muscles before bedtime, staying physically active, and ensuring you stay well-hydrated. Opt for comfortable and supportive shoes that prioritize utility.

Quickening refers to the first subtle movements you feel in your abdomen, typically around the midpoint of your pregnancy, usually around 20 weeks. There’s no need to worry if you haven’t felt these movements yet.
Some women don’t experience quickening until the sixth month of pregnancy. It’s a unique and individual experience, so the timing can vary for different women.

Dizziness during the second trimester can result from your expanding uterus pressing against blood vessels or blood sugar and hormone fluctuations. To manage this, avoid standing for extended periods, rise slowly from sitting or lying positions, maintain regular meals and snacks, and stay well-hydrated.
Choose loose clothing and refrain from hot showers or baths. Also, avoid lying flat on your back for the rest of your pregnancy. If dizziness is accompanied by fainting, vaginal bleeding, or abdominal pain, it’s crucial to contact your doctor for guidance and evaluation.
Heartburn and constipation during pregnancy are often attributed to increased hormone progesterone levels. This hormone relaxes specific muscles, including the lower oesophagal muscle ring that usually keeps food and acids in your stomach and the muscles responsible for moving digested food through your intestines.
To alleviate heartburn, consider having more frequent, smaller meals and avoiding greasy, spicy, and acidic foods. Increase your fibre intake for constipation and stay well-hydrated to facilitate smoother digestion. Engaging in physical activity can also be beneficial in promoting regular bowel.
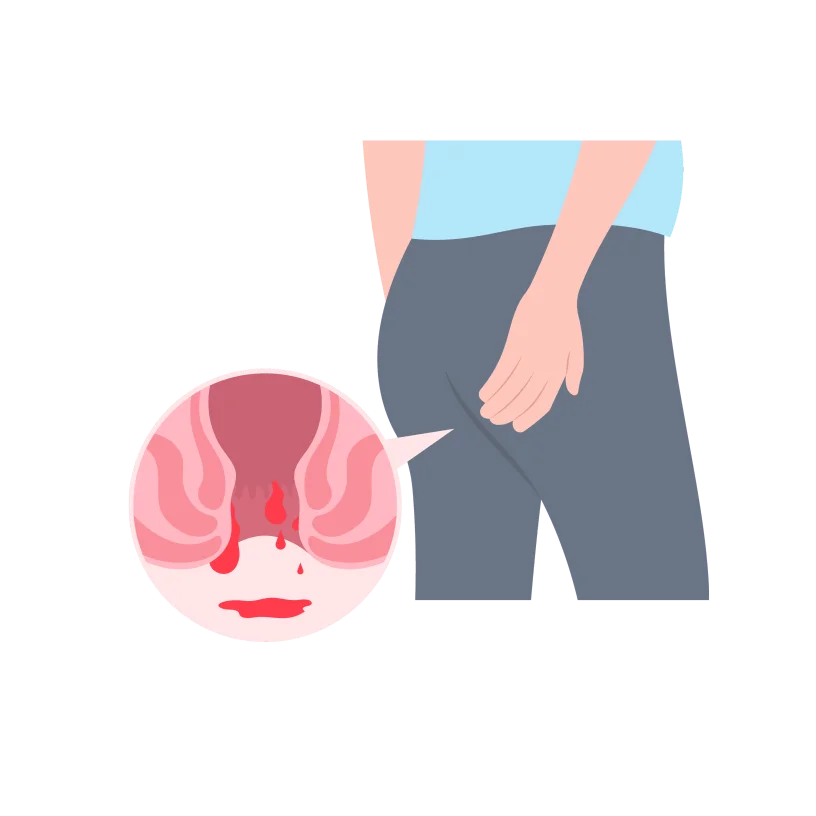
Hemorrhoids are like swollen veins around the bottom; they can become itchy and uncomfortable during pregnancy. This happens because of increased blood flow and pressure from the growing uterus.
Try sitting in a warm tub or sitz bath to ease the discomfort. You can also ask your doctor about using over-the-counter haemorrhoid ointments for relief.

Pregnancy hormones can lead to increased hair growth, making the hair on your head thicker. However, you might also notice hair in new places like your face, arms, or back. While shaving and tweezing are generally considered safe options during pregnancy.
It is advised to stay away from laser hair removal, electrolysis, waxing, or depilatories.
Headaches are common during pregnancy. Relaxation techniques like deep breathing can help. Avoid aspirin and ibuprofen, but if the headaches bother you, check with your doctor if it’s okay to take acetaminophen.
Always consult your healthcare provider before taking any medication during pregnancy.
The second trimester is a crucial phase as the fetus transitions into a baby capable of surviving outside the uterus. By the end of the second trimester, your baby will be approximately 13 to 16 inches long and weigh about 2 to 3 pounds.
The fetus kicks, moves and can turn from side to side. The fetus becomes more active and demonstrates increased mobility. It kicks, moves, and gains the ability to turn from side to side within the amniotic fluid.
Changes in the fetus’s facial features: The fetus undergoes significant changes in facial features. Initially, the eyes are positioned more to the sides but gradually move to the front of the face, and the ears shift from the neck to the sides of the head. These developments contribute to a more human-like appearance.
Additionally, the baby’s eyelids start to open, marking the beginning of eye development, and eyebrows and eyelashes become visible, enhancing the distinct features of the baby’s face.
Vernix caseosa starts to appear: A protective creamy white substance called vernix caseosa, or simply vernix, starts to appear on the fetus. This substance plays a crucial role in safeguarding the delicate fetal skin. While the vernix is gradually absorbed by the skin over time, traces of it may still be visible in babies even after birth.
This residual vernix provides additional protection for the newborn’s skin, especially in the early days after delivery.
Reflexes ( sucking and swallowing) development: The fetus develops important reflexes like swallowing and sucking. These reflexes are essential for the baby’s ability to feed and are crucial for their survival and readiness for life after birth. As the pregnancy progresses, these reflexes strengthen in preparation for the baby’s arrival.
Response to certain stimuli: In the second trimester, the fetus becomes capable of responding to specific stimuli. This responsiveness includes reactions to external sounds, movements, and even the mother’s voice. The fetus becomes increasingly sensitive to its surroundings as the nervous system develops.
These responses are early indicators of the developing sensory abilities of the baby and contribute to the intricate process of fetal growth during pregnancy.
Full development of the placenta: The placenta is fully developed by the second trimester. The placenta is a vital organ that supports the fetus during pregnancy. It facilitates the exchange of nutrients, oxygen, and waste products between the mother and the developing baby.
With its full development, the placenta ensures a stable environment for the fetus to receive the necessary nourishment and support for healthy growth until birth.
Brain development: Particularly from the fifth month onward, the fetal brain undergoes a crucial and intensive period of growth. This phase is marked by rapid development, including the formation of intricate neural connections, the growth of brain structures, and the maturation of essential functions.
Physical features become more distinct: Physical features of the fetus become more distinct. Fingernails develop on the tips of both fingers and toes and during this time, the fingers and toes fully separate. They develop distinct fingerprints and toe prints.
Hair begins to grow, and skin is covered with lanugo: Hair begins to grow on the fetus’s head, and they develop fine, downy hair known as lanugo all over their body. This hair provides some insulation for the developing baby and is usually shed before birth.
The second trimester is often a more comfortable period in pregnancy, many women experience relief from symptoms like nausea and vomiting, fatigue and the risk of miscarriage decreases.. However, complications can still arise.
Bleeding: In the second trimester, while miscarriages are less common, they can still occur, and vaginal bleeding is often the first sign. Causes may include a uterine septum, incompetent cervix, autoimmune diseases like lupus, or chromosomal abnormalities in the fetus.
Other factors for bleeding in this trimester include early labour, placental issues like placenta previa, or placental abruption. While these issues are more typical in the third trimester, they can still happen later in the second trimester.
Preterm labour: Preterm labour occurs before the 38th week and can result from factors like infections, smoking, or chronic health conditions. Risk factors include a history of preterm birth or multiple pregnancies.
Symptoms can be subtle, such as vaginal pressure or increased discharge, while more evident signs include painful contractions or vaginal bleeding.
Preterm Premature Rupture of Membranes (PPROM): This refers to the early breaking of the amniotic sac, commonly known as “water breaking,” which normally occurs during labour. This event is concerning when it happens too early in pregnancy, leading to potential infections for the baby.
In the second trimester, PPROM is particularly problematic as it can result in preterm delivery, especially between the 24th and 28th weeks, posing risks for serious long-term medical issues, notably lung disease. However, most preterm infants can fare well with appropriate intensive care nursery services.
Cervical incompetence, or cervical insufficiency: This is a condition where the cervix, the tissue connecting the vagina and the uterus, struggles to withstand the pressure from the growing uterus during pregnancy. This increased pressure can weaken the cervix, causing it to open prematurely, typically around the 20th week of pregnancy.
This condition is relatively uncommon but can lead to serious complications, including the rupture of membranes and the delivery of a very premature fetus. Unfortunately, at this early stage, the pregnancy often cannot be saved because the fetus is too premature to survive outside the uterus.
Preeclampsia: is characterized by high blood pressure, proteinuria (excessive protein in the urine), and significant oedema (swelling). It affects various systems in the body, including the placenta, which is crucial for providing nutrients to the baby.
While preeclampsia typically occurs in the third trimester for first-time pregnancies, some may experience it in the second trimester.
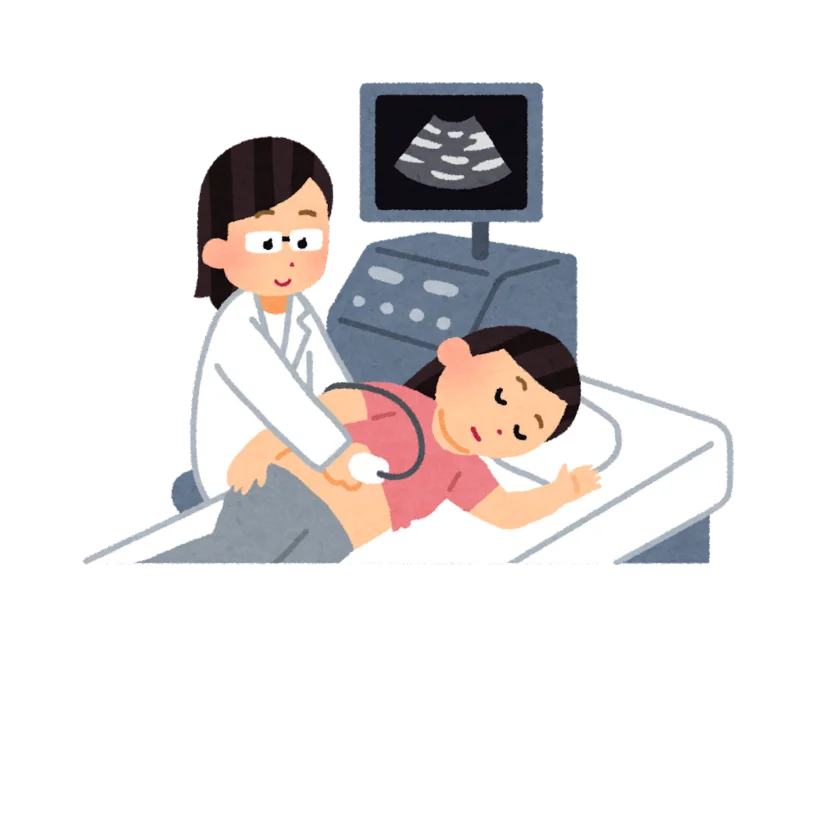
As you and your baby go through rapid growth and changes in the second trimester, your doctor will keep a closer eye on both of you. This involves routine and optional tests to check your health and your baby’s development.
Maternal blood screening: Maternal blood screening is a test that analyzes the blood for specific substances to assess the risk of congenital anomalies, commonly referred to as congenital disabilities. This screening helps identify potential risks early in pregnancy, allowing for further diagnostic evaluations or interventions if needed.
It’s a valuable tool for monitoring and addressing the well-being of both the mother and the developing baby.
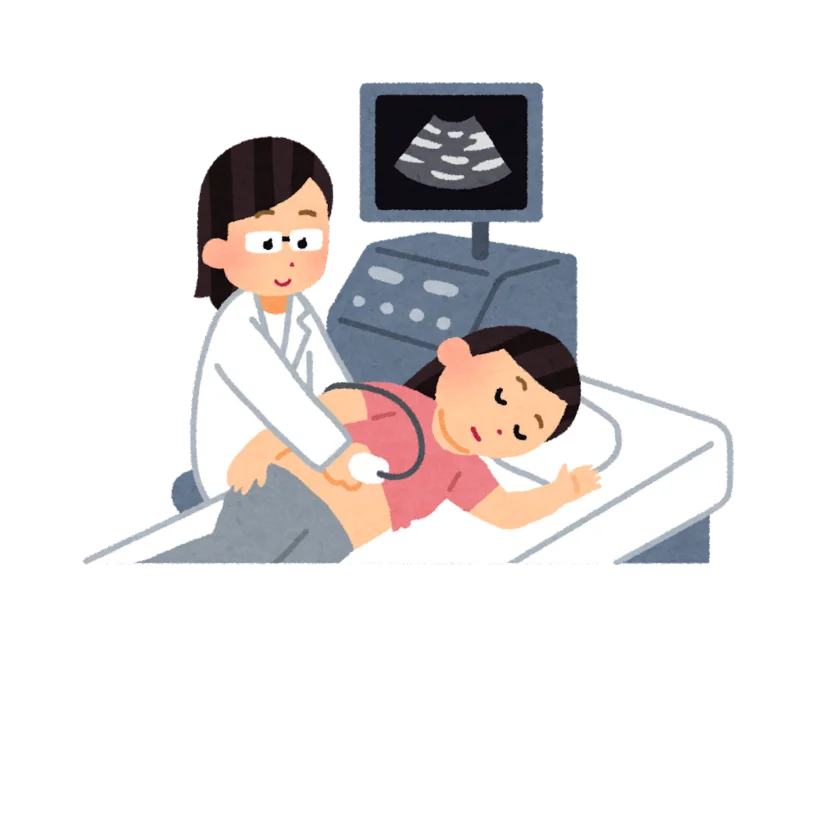
Ultrasound: During the anatomy scan ultrasound, typically between 18 to 22 weeks, you get more than just a glimpse of your baby. This detailed scan provides the first visual confirmation of your baby’s development, focusing on crucial aspects like the brain, heart, facial features, and bone structure to ensure normal development.
It’s a comprehensive check to identify any potential issues early on. Additionally, this ultrasound presents an exciting opportunity for parents to discover the gender of their baby, adding an extra layer of anticipation and connection to the pregnancy journey.
Glucose screening: Glucose screening is a test doctors recommend to check for gestational diabetes, a form of diabetes that develops during pregnancy. This screening is usually conducted between weeks 24–28 of pregnancy.
During the test, you’ll be asked to drink a sweetened solution, and then your blood sugar levels will be measured to assess how well your body processes sugar.
Amniocentesis: Amniocentesis is a medical procedure where a healthcare professional extracts a sample of amniotic fluid to assess for congenital anomalies or genetic conditions. Typically performed between weeks 15–20 of pregnancy, this procedure involves inserting a thin needle through the abdomen into the amniotic sac.
The obtained amniotic fluid contains cells from the developing baby, providing valuable information about its health. Amniocentesis is an elective test often chosen by individuals at higher risk of genetic disorders or those seeking more detailed information about the baby’s well-being.
In the second trimester, you may feel more like your pre-pregnancy self. However, there are still things to avoid.
In the second trimester, your baby undergoes significant growth, and you might be tempted to schedule a 3D or 4D ultrasound at a prenatal portrait centre. However, it’s advised to resist this urge.
Although ultrasounds are generally considered safe during pregnancy, the American College of Obstetricians and Gynecologists (ACOG) recommends that they be used only for medical reasons and conducted by qualified medical professionals, as there are concerns about the potential risks associated with extended exposure to ultrasound energy.

Hot yoga, which involves practising yoga in a heated environment, should be avoided during pregnancy. Activities that significantly raise your internal body temperature (by more than 1.5 degrees Fahrenheit) are not recommended, like hot tubs and saunas.
Although yoga is generally beneficial during pregnancy as it promotes movement and reduces stress, practising it under cooler conditions is safer to prevent overheating.
Even though your appetite may have returned during the second trimester, it’s crucial to avoid raw or undercooked foods, including seafood, eggs, and meat. These precautions are in place to reduce the risk of foodborne illnesses that could harm you and your baby.

Unpasteurized dairy and juices are products that have not undergone pasteurization. Pasteurization involves heating the food or beverage to a specific temperature to kill harmful bacteria and pathogens.
Consuming unpasteurized products during pregnancy poses a risk of bacterial infections, such as those caused by harmful microorganisms like Salmonella or E. coli. To ensure food safety for both you and your baby, it’s recommended to choose pasteurized dairy products and juices.
Avoid lying flat on your back during pregnancy to prevent the weight of your uterus and baby from putting too much pressure on your back, intestines, and the main vein that transports blood from your lower body to your heart. This can affect blood flow and cause discomfort. Choose other positions for sleeping or exercising to relieve this pressure.
In the second trimester, your baby undergoes significant growth, and you might be tempted to schedule a 3D or 4D ultrasound at a prenatal portrait centre. However, it’s advised to resist this urge.
Although ultrasounds are generally considered safe during pregnancy, the American College of Obstetricians and Gynecologists (ACOG) recommends that they be used only for medical reasons and conducted by qualified medical professionals, as there are concerns about the potential risks associated with extended exposure to ultrasound energy.

Hot yoga, which involves practising yoga in a heated environment, should be avoided during pregnancy. Activities that significantly raise your internal body temperature (by more than 1.5 degrees Fahrenheit) are not recommended, like hot tubs and saunas.
Although yoga is generally beneficial during pregnancy as it promotes movement and reduces stress, practising it under cooler conditions is safer to prevent overheating.
Even though your appetite may have returned during the second trimester, it’s crucial to avoid raw or undercooked foods, including seafood, eggs, and meat. These precautions are in place to reduce the risk of foodborne illnesses that could harm you and your baby.

Unpasteurized dairy and juices are products that have not undergone pasteurization. Pasteurization involves heating the food or beverage to a specific temperature to kill harmful bacteria and pathogens.
Consuming unpasteurized products during pregnancy poses a risk of bacterial infections, such as those caused by harmful microorganisms like Salmonella or E. coli. To ensure food safety for both you and your baby, it’s recommended to choose pasteurized dairy products and juices.
Avoid lying flat on your back during pregnancy to prevent the weight of your uterus and baby from putting too much pressure on your back, intestines, and the main vein that transports blood from your lower body to your heart. This can affect blood flow and cause discomfort. Choose other positions for sleeping or exercising to relieve this pressure.
Once you’re in your second trimester, things might get easier for the next three months. However, certain symptoms can prompt you to contact your doctor.
Always contact your healthcare provider if you have any doubts or concerns. They can offer reassurance, conduct necessary tests, and provide appropriate guidance tailored to your situation. Trust your instincts and listen to your body. If something doesn’t feel right, don’t hesitate to seek help promptly.
The second trimester typically starts around week 13 of pregnancy and lasts until the end of week 26.
As your belly grows in the second trimester, lying face down becomes uncomfortable, and sleeping on your back can put pressure on muscles and the spine. Opting for a side-sleeping position with your knees bent is generally considered the most comfortable and safe during this stage of pregnancy.
In the second trimester, the excitement of feeling your baby move begins, often described as gentle flutters in your abdomen. Distinguishing these flutters from gas bubbles can be tricky, but around 20 to 22 weeks, you may better identify your baby’s kicks. If you don’t feel movement initially, the placenta’s position at the front of your uterus might be acting as a barrier. As your baby grows, you’ll likely start sensing movements more distinctly.
Yes, it’s generally safe to have intercourse during the second trimester of pregnancy. However, it’s crucial to communicate with your healthcare provider about any concerns or specific conditions you may have. In most cases, if your pregnancy is progressing without complications, intimacy is considered safe during this stage.
Certain vaccines are recommended during pregnancy to protect you and your baby. The flu vaccine is recommended to safeguard against influenza, and the Tdap vaccine is suggested to provide immunity against tetanus, diphtheria, and pertussis (whooping cough).
These vaccines help prevent potential complications during pregnancy and protect your newborn in the early months of life. It’s essential to consult with your healthcare provider to discuss the appropriate vaccinations based on your health circumstances and the specific recommendations for your region.
As your body adapts to hormonal changes and your uterus grows in the second trimester, the pressure on your bladder decreases, relieving frequent urination. The uterus shifts higher in the abdomen, reducing the urge to pee as often.
However, as you enter the third trimester, increased pressure on the bladder may resume, leading to more bathroom trips. It’s important to note that feeling the need to urinate frequently is common at any stage of pregnancy. If you encounter pain during urination, notice unusual urine characteristics, or experience severe incontinence, consult your doctor for guidance.
The second trimester typically starts around week 13 of pregnancy and lasts until the end of week 26.
As your belly grows in the second trimester, lying face down becomes uncomfortable, and sleeping on your back can put pressure on muscles and the spine. Opting for a side-sleeping position with your knees bent is generally considered the most comfortable and safe during this stage of pregnancy.
In the second trimester, the excitement of feeling your baby move begins, often described as gentle flutters in your abdomen. Distinguishing these flutters from gas bubbles can be tricky, but around 20 to 22 weeks, you may better identify your baby’s kicks.
If you don’t feel movement initially, the placenta’s position at the front of your uterus might be acting as a barrier. As your baby grows, you’ll likely start sensing movements more distinctly.
Yes, it’s generally safe to have intercourse during the second trimester of pregnancy. However, it’s crucial to communicate with your healthcare provider about any concerns or specific conditions you may have. In most cases, if your pregnancy is progressing without complications, intimacy is considered safe during this stage.
Certain vaccines are recommended during pregnancy to protect you and your baby. The flu vaccine is recommended to safeguard against influenza, and the Tdap vaccine is suggested to provide immunity against tetanus, diphtheria, and pertussis (whooping cough).
These vaccines help prevent potential complications during pregnancy and protect your newborn in the early months of life. It’s essential to consult with your healthcare provider to discuss the appropriate vaccinations based on your health circumstances and the specific recommendations for your region.
As your body adapts to hormonal changes and your uterus grows in the second trimester, the pressure on your bladder decreases, relieving frequent urination. The uterus shifts higher in the abdomen, reducing the urge to pee as often.
However, as you enter the third trimester, increased pressure on the bladder may resume, leading to more bathroom trips. It’s important to note that feeling the need to urinate frequently is common at any stage of pregnancy.
If you encounter pain during urination, notice unusual urine characteristics, or experience severe incontinence, consult your doctor for guidance.
1. American College of Obstetricians and Gynecologists: Ultrasound Examination.
2. Centers for Disease Control and Prevention. Gestational Diabetes.
3. Johns Hopkins Medicine. The second Trimester.
4. Healthline. Second Trimester Pregnancy Complications.
5. Kumar, A., Basra, M., Begum, N., Rani, V., Prasad, S., Lamba, A.K., Verma, M., Agarwal, S. and Sharma, S., 2013. Association of maternal periodontal health with adverse pregnancy outcome. Journal of Obstetrics and Gynaecology Research, 39(1), pp.40-45.
6. MedicalNewsToday: Everything to know about the second trimester.
7. WebMD: Second Trimester of Pregnancy.
© Mindsmaking 2024