Menu

Congratulations, you’ve reached the final stretch of your pregnancy! The third trimester is undeniably exciting and suspenseful as you eagerly await the arrival of your little one. It’s natural to be impatient, but rest assured, soon you’ll be holding your newborn in your arms.
This trimester can pose physical and emotional challenges as your baby grows and changes position, and finding comfort might become more challenging. However, maintaining a positive outlook is key as you anticipate the end of your pregnancy journey. Soon, you’ll embrace the joy of holding your baby in your arms.
As your pregnancy advances, your baby’s movements become more pronounced. While these sensations are exciting, they may also bring about increased discomfort. Alongside these movements, you may experience various signs and symptoms as your body adjusts to the changes,
Pregnancy hormones relax connective tissue, especially in the pelvic area, affecting bone stability and contributing to back discomfort in the third trimester. To alleviate this, opt for chairs with good back support when sitting, exercise regularly, and wear low-heeled shoes with proper arch support.
If you experience severe or persistent pain, contacting your healthcare provider for guidance is crucial.
These are mild, irregular sensations of tightness in your abdomen. They commonly occur in the afternoon or evening, especially after physical activity or sex. As you approach your due date, these contractions may increase in frequency and intensity.
While these contractions are usually harmless, it’s essential to contact your healthcare provider if they become regular and steadily stronger, as this could indicate preterm labour or other concerns that need attention.
During the third trimester, abdominal achiness is common as your growing baby occupies more space in your abdomen. This can lead to discomfort and difficulty finding a comfortable position, particularly when sleeping at night.
The pressure from your expanding belly may also make it challenging to take deep breaths.
In the third trimester, your breasts continue to change in preparation for breastfeeding. As you approach your due date, you might observe a yellowish fluid, colostrum, leaking from your nipples.
Colostrum is rich in nutrients and is the first nourishment for your baby during the days after birth.
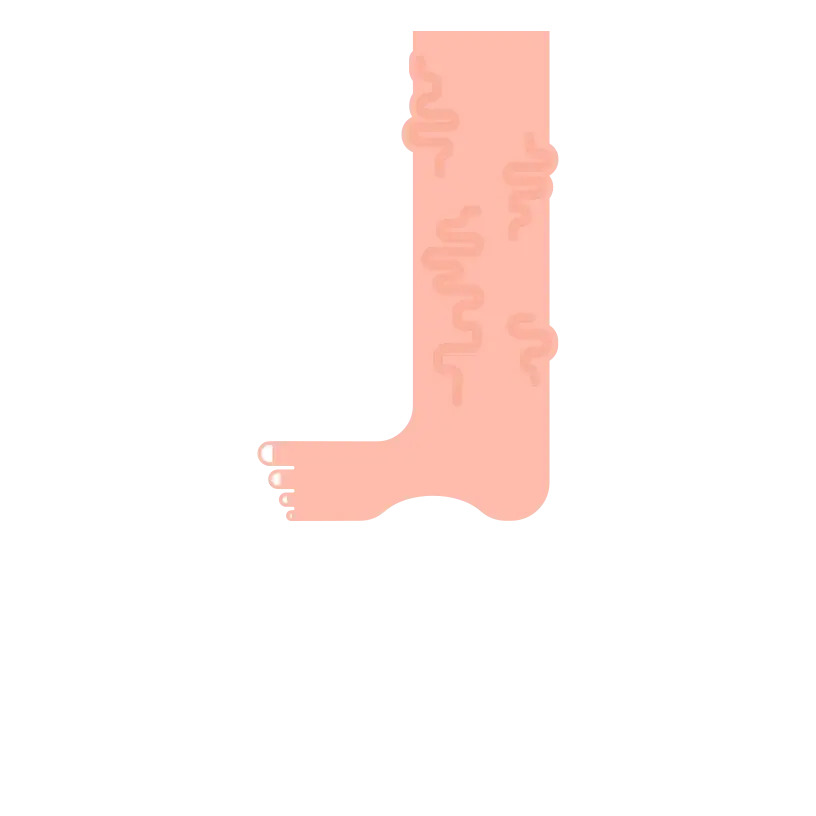
Swelling, or oedema, is common in the third trimester due to increased fluid retention and pressure on blood vessels. It often affects the ankles, feet, and hands.
To minimize swelling, stay hydrated, elevate your legs when possible, and avoid standing or sitting for extended periods.
If you notice sudden or severe swelling, especially in the face, contact your healthcare provider, as it could indicate a more serious condition.
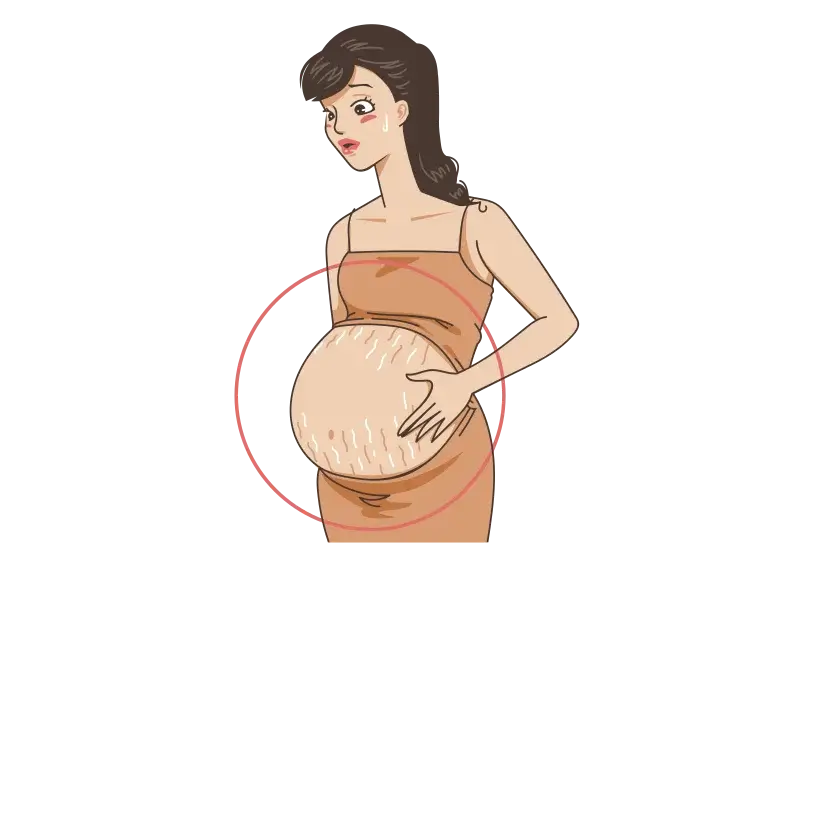
it’s common to develop stretch marks on areas like your breasts, buttocks, abdomen, or thighs. These marks can appear as reddish or purplish streaks on the skin and result from stretching your skin during pregnancy.
While Stretch marks are common in pregnancy, keeping your skin well-moisturized may help minimize their severity.
Increased circulation to support your growing baby can lead to the appearance of tiny red veins, known as spider veins, on your skin. While they may worsen during this trimester, they often fade after childbirth.
Pressure from your growing baby can also result in swollen, blue, or purple surface veins, known as varicose veins. Thankfully, these typically improve a few months post-delivery.
To manage or prevent worsening varicose veins, consider regular movement throughout the day, wearing support hose, and propping up your legs when sitting for extended periods.

Shortness of breath is common in the third trimester due to the expanding uterus putting pressure on your diaphragm. As a result, there’s less room for your lungs to expand fully. This can make breathing feel more challenging.
Try sitting up straight, sleeping with extra pillows, and taking things slower to ease this discomfort.

In the third trimester, sciatica, characterized by pain radiating along the sciatic nerve, can occur due to pressure from the growing uterus on the lower back and pelvic region. This can lead to discomfort, tingling, or numbness along the back of the leg.
While practices like yoga, massage, or physical therapy can offer relief, the pain typically diminishes after childbirth.
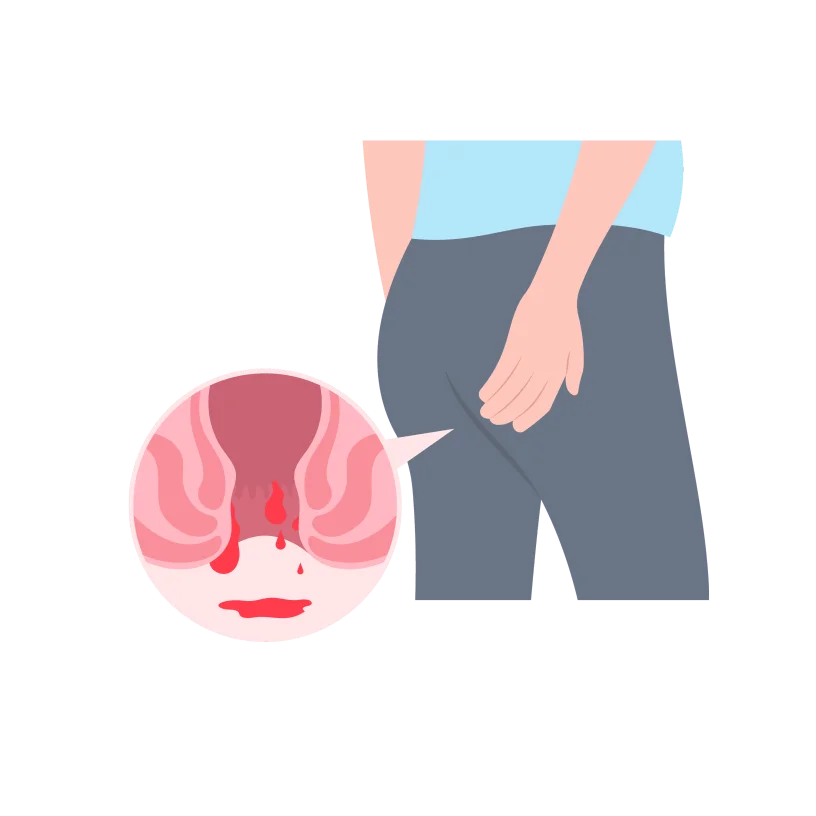
Hemorrhoids, which are essentially varicose veins around the anus, tend to enlarge during pregnancy due to increased blood flow and added pressure from the growing uterus. This can lead to itching and discomfort.
To manage haemorrhoids, consider maintaining a high-fibre diet, staying hydrated, and avoiding prolonged periods of sitting or straining during bowel movements.

Heartburn and constipation are common discomforts during the third trimester of pregnancy. The growing uterus puts pressure on the digestive organs, leading to heartburn, characterized by a burning sensation in the chest.
Constipation may occur due to hormonal changes slowing down bowel movements. To manage heartburn, consider smaller, more frequent meals and avoid spicy or acidic foods. For constipation, focus on a high-fibre diet, stay hydrated, and engage in regular physical activity.

The pressure from your growing baby’s head on your bladder can lead to more frequent bathroom visits, including at night. You might also notice urine leakage when coughing, sneezing, laughing, or exercising.
To manage this, respond promptly to urges and ensure you empty your bladder fully. Minimize fluid intake before bedtime to reduce nighttime bathroom visits, and consider using a panty liner for any leakage.
If you experience pain or burning during urination, it’s crucial to inform your doctor, as these could be signs of a urinary tract infection.
As your body works hard to support the growing baby, hormonal changes, increased weight, and disrupted sleep patterns contribute to feeling more tired.
To manage fatigue, prioritize rest, take short naps when needed, maintain a balanced diet, and engage in light exercise.

In the third trimester, an increase in vaginal discharge is common. If the flow becomes heavy enough to soak through panty liners, it’s advisable to contact your doctor.
As you approach your delivery date, you might notice a thick, clear, or slightly blood-tinged discharge – this is your mucus plug, indicating your cervix is dilating in preparation for labour.
If you experience a sudden rush of fluid could be a sign that your water has broken. In such cases, you must call your doctor promptly for guidance and appropriate next steps.

In the third trimester, feeling clumsy or off-balance is not uncommon, and it can be attributed, in part, to the additional weight gain in the belly area. This weight distribution makes it more challenging to maintain balance, and you may be dropping things or feeling less steady.
The body’s changing centre of gravity due to the growing baby contributes to this sense of clumsiness.
Experiencing vivid dreams during the third trimester of pregnancy is common and often linked to hormonal changes, increased emotional intensity, and disrupted sleep patterns. As your body prepares for labour and you navigate the anticipation of parenthood, these factors can contribute to more vivid and memorable dreams.
While this phenomenon is generally considered normal, if your dreams cause distress or impact your sleep quality, practising relaxation techniques before bedtime and maintaining a consistent sleep routine is helpful.
Lightning crotch” refers to sharp or shooting pains in the pelvic area during the third trimester of pregnancy. This discomfort is often caused by the baby’s head engaging in the pelvis, putting pressure on nerves and ligaments.
While it can be a normal part of the baby’s descent into the birth canal, if the pain is severe or persistent, it’s advisable to discuss it with your healthcare provider.
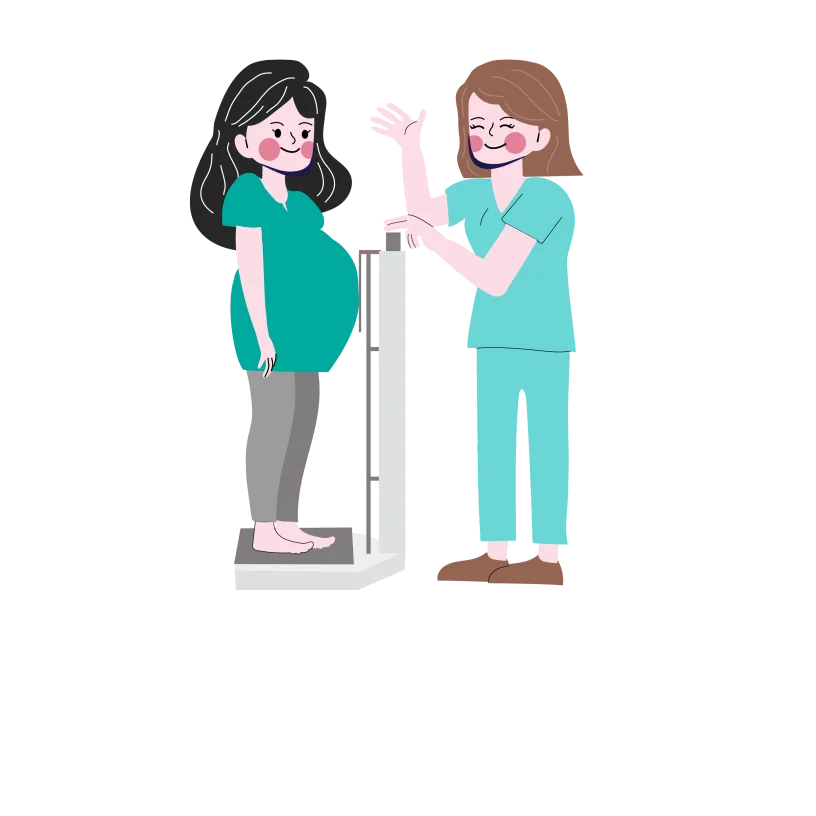
Weight gain in the third trimester of pregnancy is normal. The amount of weight gained can vary among individuals. Still, on average, it’s recommended for women with a healthy pre-pregnancy weight to gain around 1 pound per week during the third trimester.
This weight gain is primarily attributed to the baby’s growth, increased amniotic fluid, and additional support structures.
Pregnancy hormones relax connective tissue, especially in the pelvic area, affecting bone stability and contributing to back discomfort in the third trimester. To alleviate this, opt for chairs with good back support when sitting, exercise regularly, and wear low-heeled shoes with proper arch support.
If you experience severe or persistent pain, contacting your healthcare provider for guidance is crucial.
These are mild, irregular sensations of tightness in your abdomen. They commonly occur in the afternoon or evening, especially after physical activity or sex. As you approach your due date, these contractions may increase in frequency and intensity.
While these contractions are usually harmless, it’s essential to contact your healthcare provider if they become regular and steadily stronger, as this could indicate preterm labour or other concerns that need attention.
During the third trimester, abdominal achiness is common as your growing baby occupies more space in your abdomen. This can lead to discomfort and difficulty finding a comfortable position, particularly when sleeping at night.
The pressure from your expanding belly may also make it challenging to take deep breaths.
In the third trimester, your breasts continue to change in preparation for breastfeeding. As you approach your due date, you might observe a yellowish fluid, colostrum, leaking from your nipples.
Colostrum is rich in nutrients and is the first nourishment for your baby during the days after birth.
Swelling, or oedema, is common in the third trimester due to increased fluid retention and pressure on blood vessels. It often affects the ankles, feet, and hands.
To minimize swelling, stay hydrated, elevate your legs when possible, and avoid standing or sitting for extended periods.
If you notice sudden or severe swelling, especially in the face, contact your healthcare provider, as it could indicate a more serious condition.
It’s common to develop stretch marks on areas like your breasts, buttocks, abdomen, or thighs. These marks can appear as reddish or purplish streaks on the skin and result from stretching your skin during pregnancy.
While Stretch marks are common in pregnancy, keeping your skin well-moisturized may help minimize their severity.
Increased circulation to support your growing baby can lead to the appearance of tiny red veins, known as spider veins, on your skin. While they may worsen during this trimester, they often fade after childbirth.
Pressure from your growing baby can also result in swollen, blue, or purple surface veins, known as varicose veins. Thankfully, these typically improve a few months post-delivery.
To manage or prevent worsening varicose veins, consider regular movement throughout the day, wearing support hose, and propping up your legs when sitting for extended periods.

Shortness of breath is common in the third trimester due to the expanding uterus putting pressure on your diaphragm. As a result, there’s less room for your lungs to expand fully. This can make breathing feel more challenging.
Try sitting up straight, sleeping with extra pillows, and taking things slower to ease this discomfort.

In the third trimester, sciatica, characterized by pain radiating along the sciatic nerve, can occur due to pressure from the growing uterus on the lower back and pelvic region. This can lead to discomfort, tingling, or numbness along the back of the leg.
While practices like yoga, massage, or physical therapy can offer relief, the pain typically diminishes after childbirth.
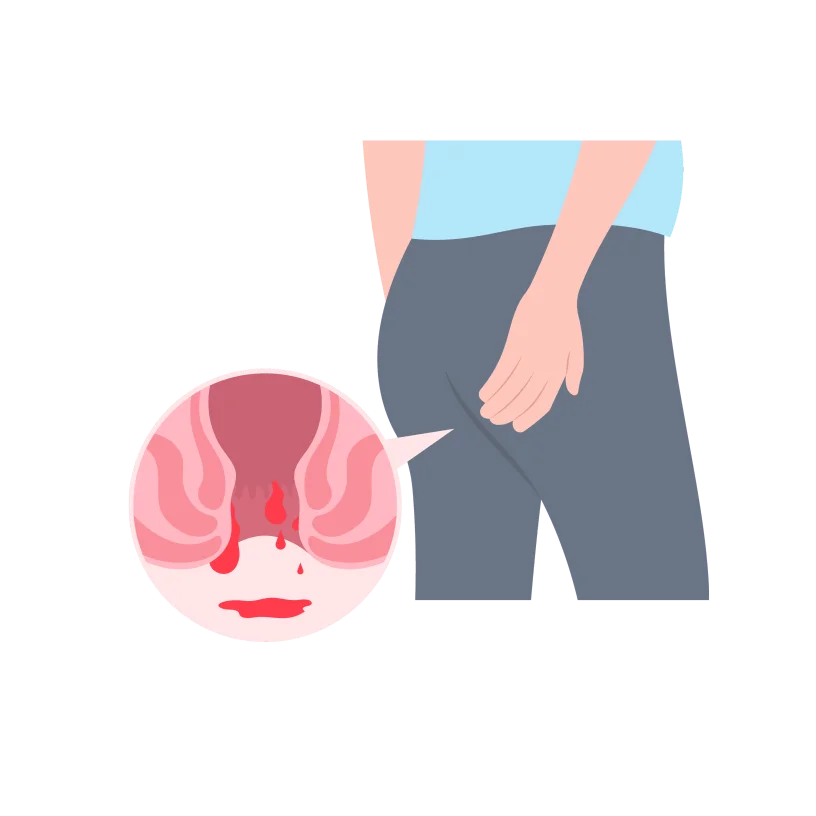
Hemorrhoids, which are essentially varicose veins around the anus, tend to enlarge during pregnancy due to increased blood flow and added pressure from the growing uterus. This can lead to itching and discomfort.
To manage haemorrhoids, consider maintaining a high-fibre diet, staying hydrated, and avoiding prolonged periods of sitting or straining during bowel movements.

Heartburn and constipation are common discomforts during the third trimester of pregnancy. The growing uterus puts pressure on the digestive organs, leading to heartburn, characterized by a burning sensation in the chest.
Constipation may occur due to hormonal changes slowing down bowel movements. To manage heartburn, consider smaller, more frequent meals and avoid spicy or acidic foods. For constipation, focus on a high-fibre diet, stay hydrated, and engage in regular physical activity.

The pressure from your growing baby’s head on your bladder can lead to more frequent bathroom visits, including at night. You might also notice urine leakage when coughing, sneezing, laughing, or exercising.
To manage this, respond promptly to urges and ensure you empty your bladder fully. Minimize fluid intake before bedtime to reduce nighttime bathroom visits, and consider using a panty liner for any leakage.
If you experience pain or burning during urination, it’s crucial to inform your doctor, as these could be signs of a urinary tract infection.
As your body works hard to support the growing baby, hormonal changes, increased weight, and disrupted sleep patterns contribute to feeling more tired.
To manage fatigue, prioritize rest, take short naps when needed, maintain a balanced diet, and engage in light exercise.

In the third trimester, an increase in vaginal discharge is common. If the flow becomes heavy enough to soak through panty liners, it’s advisable to contact your doctor.
As you approach your delivery date, you might notice a thick, clear, or slightly blood-tinged discharge – this is your mucus plug, indicating your cervix is dilating in preparation for labour.
If you experience a sudden rush of fluid could be a sign that your water has broken. In such cases, you must call your doctor promptly for guidance and appropriate next steps.

In the third trimester, feeling clumsy or off-balance is not uncommon, and it can be attributed, in part, to the additional weight gain in the belly area. This weight distribution makes it more challenging to maintain balance, and you may be dropping things or feeling less steady.
The body’s changing centre of gravity due to the growing baby contributes to this sense of clumsiness.
Experiencing vivid dreams during the third trimester of pregnancy is common and often linked to hormonal changes, increased emotional intensity, and disrupted sleep patterns. As your body prepares for labour and you navigate the anticipation of parenthood, these factors can contribute to more vivid and memorable dreams.
While this phenomenon is generally considered normal, if your dreams cause distress or impact your sleep quality, practising relaxation techniques before bedtime and maintaining a consistent sleep routine is helpful.
Lightning crotch” refers to sharp or shooting pains in the pelvic area during the third trimester of pregnancy. This discomfort is often caused by the baby’s head engaging in the pelvis, putting pressure on nerves and ligaments.
While it can be a normal part of the baby’s descent into the birth canal, if the pain is severe or persistent, it’s advisable to discuss it with your healthcare provider.
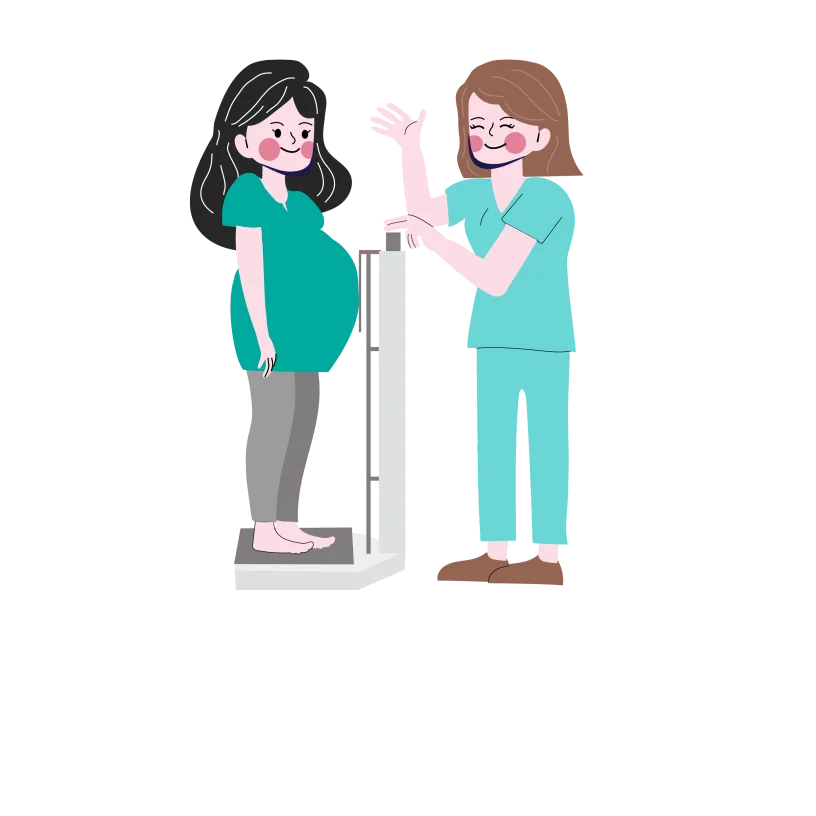
Weight gain in the third trimester of pregnancy is normal. The amount of weight gained can vary among individuals. Still, on average, it’s recommended for women with a healthy pre-pregnancy weight to gain around 1 pound per week during the third trimester.
This weight gain is primarily attributed to the baby’s growth, increased amniotic fluid, and additional support structures.
In the third trimester, your baby undergoes significant growth and development. As the lungs mature, your baby typically positions its head down in preparation for birth. By the end of this trimester, your baby reaches an average length of 19 to 21 inches and weighs between 6 to 9 pounds.
Baby can see and hear: In the third trimester, your baby’s eyes and ears are developing, allowing them to see and hear to some extent. Although their vision isn’t crystal clear yet, they can detect changes in light.
They can also hear sounds from the outside world, like your voice and other noises. So, talking to your baby or playing music during this time can be a way to start connecting with them even before they’re born.
The brain continues to develop: In the third trimester, your baby’s brain experiences a remarkable surge in growth, showcasing some impressive developmental skills. This includes the ability to blink, indicating the formation and function of the eyes.
Moreover, your baby starts dreaming during this stage, a fascinating aspect of brain activity. Additionally, the brain is working on regulating body temperature, a crucial skill for life outside the womb.
Baby’s bones are fully formed: By around week 32 of pregnancy, your baby’s bones are fully formed, providing a sturdy skeletal structure. Your baby’s body begins to store essential minerals such as iron and calcium, which are crucial for overall growth and development.
The bones of your baby’s skull remain soft to facilitate the birthing process. This flexibility is essential for the baby to navigate and pass through the narrow birth canal during delivery.
Baby’s head descends into the pelvis: Around the 36th week of pregnancy, the baby should be in a head-down position and move down into the lower part of the pelvis. This is called “lightening.” It’s a sign that the baby is getting ready for birth. When this happens, it can make breathing easier for you because the baby’s head is no longer pressing up against the lungs. Lightening is a normal part of the final weeks of pregnancy as the body prepares for labour.
Lanugo disappears: Between 38 to 40 weeks of pregnancy, the fetus undergoes changes, and the lanugo, which is the fine, soft hair covering the body and limbs, has almost completely disappeared. Lanugo initially serves the purpose of helping regulate the baby’s body temperature in the womb.
As your baby nears full-term development, the decrease in lanugo marks a natural part of the maturation process, making way for their readiness for life outside the womb.
Baby’s lungs mature and are ready to function independently: Between 38 to 40 weeks of pregnancy, the baby’s lungs have typically matured completely. This maturation is a crucial milestone for the baby’s ability to breathe independently after birth.
The lungs’ full development involves the production of surfactant, a substance that helps the air sacs stay open and prevents them from collapsing.
The matured lungs are better equipped to handle the transition from the fluid-filled environment of the womb to breathing air in the outside world.
Gestational diabetes arises due to hormonal changes during pregnancy, making it challenging for the body to utilize insulin effectively. Insulin plays a crucial role in lowering blood sugar levels; when it fails, it results in elevated glucose levels.
Interestingly, most women with gestational diabetes don’t experience noticeable symptoms. While the condition is generally not harmful to the mother, however, it can present challenges for the baby.
Excessive fetal growth, known as macrosomia, increases the chances of cesarean delivery and raises the risk of birth injuries.
When glucose levels are well-controlled through proper management, the likelihood of macrosomia decreases. Regular monitoring, dietary adjustments, and, if necessary, medication can contribute to better control of gestational diabetes and reduce potential risks for both the mother and the baby.
Preeclampsia is a serious pregnancy condition that occurs after 20 weeks, posing risks for both the mother and baby. About 5 to 8 percent of women may experience it, with higher risks for teenagers, women 35 and older, and first-time mothers, especially African American women.
Symptoms of preeclampsia include high blood pressure, protein in the urine, sudden weight gain, and swelling. Regular prenatal visits are crucial for early detection, as screenings can identify warning signs like elevated blood pressure and protein in the urine.
If preeclampsia is left untreated, it can lead to severe complications such as seizures, kidney failure, and, in severe cases, death for both the mother and the baby.
Rupture of membranes, commonly known as “water breaking,” is a natural occurrence during childbirth. It indicates that the amniotic sac, which surrounds the baby, has ruptured, releasing amniotic fluid.
While it’s typical for the sac to break during labour, if this happens too early, it can result in significant complications known as preterm or premature rupture of membranes (PROM). The cause of PROM is not always clear, but infections of the amniotic membranes can contribute, and genetic factors may also play a role.
Preterm rupture of membranes can lead to preterm birth, posing risks to the baby’s health and development. Monitoring and timely medical intervention are crucial in cases of PROM to reduce potential complications.
Placenta previa is a condition where the placenta blocks the cervix, increasing the risk of serious bleeding during pregnancy. It’s more common in women with a history of cesarean delivery, uterine surgery, or smoking.
Symptoms of Placenta previa include painless, sudden, and profuse bright red vaginal bleeding after the 28th week of pregnancy. Diagnosis is typically done through ultrasound. Treatment depends on factors like fetal age and bleeding severity.
Immediate cesarean delivery is necessary in critical situations, while in less severe cases, delivery may be delayed to allow more time for fetal growth.
Placental abruption is a rare condition where the placenta separates from the uterus before labour, occurring in about 1 per cent of pregnancies. It poses serious risks, including fetal death, significant bleeding, and shock for the mother.
Risk factors include advanced maternal age, substance use, diabetes, high blood pressure, multiple pregnancies, and trauma to the stomach.
Symptoms of Placenta abruption vary, with some women experiencing heavy bleeding and severe pain while others may have no bleeding. Rapid cesarean delivery is often necessary, and in cases of excessive bleeding, a blood transfusion may be required.
This occurs when a baby doesn’t grow as expected during a stage of pregnancy. It can be symmetrical or asymmetrical, with factors like maternal anaemia, chronic renal disease, and placenta issues contributing.
IUGR babies may struggle with labour stress, have less body fat, and face challenges after birth. Ultrasounds measure fetal growth and estimate weight and ongoing monitoring assesses weight gain. If growth issues persist, doctors may recommend induction or cesarean delivery. Most IUGR babies develop normally after birth, catching up in growth by age two.
Monitoring, timely intervention, and post-birth care are crucial for positive outcomes.
This occurs when a woman delivers at 42 weeks or later, affecting about 7 per cent of pregnancies. The cause is unclear, but hormonal and hereditary factors are suspected. Incorrect due date calculations or irregular menstrual cycles can contribute.
While generally not dangerous for the mother, concerns arise for the fetus due to potential issues with the placenta’s effectiveness after 41 weeks, leading to decreased amniotic fluid (oligohydramnios). This can compress the umbilical cord, reducing oxygen supply and posing a risk of sudden fetal death.
Monitoring from 41 weeks includes fetal heart rate and amniotic fluid measurements. If abnormalities are detected, induction is recommended; otherwise, spontaneous labour is awaited until around 42 to 43 weeks.
Meconium aspiration syndrome (MAS) is associated with meconium, a fetus’ bowel movement, in the amniotic fluid. This condition is a significant cause of severe illness and mortality in newborns, affecting approximately 5 to 10 per cent of births.
MAS is more likely to occur when the fetus experiences stress during labour, particularly in cases of post-term pregnancies.
Malpresentation, including breech (bottom or feet first) and transverse lie (sideways), occurs in a small percentage of full-term pregnancies. The external cephalic version, a technique to turn the fetus to a head-down position, is attempted around 37 to 38 weeks. This procedure carries rare risks, and if successful, spontaneous labour or induced labour may follow. If unsuccessful, the doctor may reattempt or discuss the best delivery method, considering factors like vaginal or cesarean delivery.
For breech presentations, measurements of the birth canal and fetal weight are obtained for potential vaginal deliveries. However, if the baby remains breech or is in a transverse lie, a cesarean delivery is typically recommended.
Gestational diabetes arises due to hormonal changes during pregnancy, making it challenging for the body to utilize insulin effectively. Insulin plays a crucial role in lowering blood sugar levels; when it fails, it results in elevated glucose levels.
Interestingly, most women with gestational diabetes don’t experience noticeable symptoms. While the condition is generally not harmful to the mother, however, it can present challenges for the baby.
Excessive fetal growth, known as macrosomia, increases the chances of cesarean delivery and raises the risk of birth injuries.
When glucose levels are well-controlled through proper management, the likelihood of macrosomia decreases. Regular monitoring, dietary adjustments, and, if necessary, medication can contribute to better control of gestational diabetes and reduce potential risks for both the mother and the baby.
Preeclampsia is a serious pregnancy condition that occurs after 20 weeks, posing risks for both the mother and baby. About 5 to 8 percent of women may experience it, with higher risks for teenagers, women 35 and older, and first-time mothers, especially African American women.
Symptoms of preeclampsia include high blood pressure, protein in the urine, sudden weight gain, and swelling. Regular prenatal visits are crucial for early detection, as screenings can identify warning signs like elevated blood pressure and protein in the urine.
If preeclampsia is left untreated, it can lead to severe complications such as seizures, kidney failure, and, in severe cases, death for both the mother and the baby.
Rupture of membranes, commonly known as “water breaking,” is a natural occurrence during childbirth. It indicates that the amniotic sac, which surrounds the baby, has ruptured, releasing amniotic fluid.
While it’s typical for the sac to break during labour, if this happens too early, it can result in significant complications known as preterm or premature rupture of membranes (PROM). The cause of PROM is not always clear, but infections of the amniotic membranes can contribute, and genetic factors may also play a role.
Preterm rupture of membranes can lead to preterm birth, posing risks to the baby’s health and development. Monitoring and timely medical intervention are crucial in cases of PROM to reduce potential complications.
Placenta previa is a condition where the placenta blocks the cervix, increasing the risk of serious bleeding during pregnancy. It’s more common in women with a history of cesarean delivery, uterine surgery, or smoking.
Symptoms of Placenta previa include painless, sudden, and profuse bright red vaginal bleeding after the 28th week of pregnancy. Diagnosis is typically done through ultrasound. Treatment depends on factors like fetal age and bleeding severity.
Immediate cesarean delivery is necessary in critical situations, while in less severe cases, delivery may be delayed to allow more time for fetal growth.
Placental abruption is a rare condition where the placenta separates from the uterus before labour, occurring in about 1 per cent of pregnancies. It poses serious risks, including fetal death, significant bleeding, and shock for the mother.
Risk factors include advanced maternal age, substance use, diabetes, high blood pressure, multiple pregnancies, and trauma to the stomach.
Symptoms of Placenta abruption vary, with some women experiencing heavy bleeding and severe pain while others may have no bleeding. Rapid cesarean delivery is often necessary, and in cases of excessive bleeding, a blood transfusion may be required.
This occurs when a baby doesn’t grow as expected during a stage of pregnancy. It can be symmetrical or asymmetrical, with factors like maternal anaemia, chronic renal disease, and placenta issues contributing.
IUGR babies may struggle with labour stress, have less body fat, and face challenges after birth. Ultrasounds measure fetal growth and estimate weight and ongoing monitoring assesses weight gain. If growth issues persist, doctors may recommend induction or cesarean delivery. Most IUGR babies develop normally after birth, catching up in growth by age two.
Monitoring, timely intervention, and post-birth care are crucial for positive outcomes.
This occurs when a woman delivers at 42 weeks or later, affecting about 7 per cent of pregnancies. The cause is unclear, but hormonal and hereditary factors are suspected. Incorrect due date calculations or irregular menstrual cycles can contribute.
While generally not dangerous for the mother, concerns arise for the fetus due to potential issues with the placenta’s effectiveness after 41 weeks, leading to decreased amniotic fluid (oligohydramnios). This can compress the umbilical cord, reducing oxygen supply and posing a risk of sudden fetal death.
Monitoring from 41 weeks includes fetal heart rate and amniotic fluid measurements. If abnormalities are detected, induction is recommended; otherwise, spontaneous labour is awaited until around 42 to 43 weeks.
Meconium aspiration syndrome (MAS) is associated with meconium, a fetus’ bowel movement, in the amniotic fluid. This condition is a significant cause of severe illness and mortality in newborns, affecting approximately 5 to 10 per cent of births.
MAS is more likely to occur when the fetus experiences stress during labour, particularly in cases of post-term pregnancies.
Malpresentation, including breech (bottom or feet first) and transverse lie (sideways), occurs in a small percentage of full-term pregnancies. The external cephalic version, a technique to turn the fetus to a head-down position, is attempted around 37 to 38 weeks.
This procedure carries rare risks, and if successful, spontaneous labour or induced labour may follow. If unsuccessful, the doctor may reattempt or discuss the best delivery method, considering factors like vaginal or cesarean delivery.
For breech presentations, measurements of the birth canal and fetal weight are obtained for potential vaginal deliveries. However, if the baby remains breech or is in a transverse lie, a cesarean delivery is typically recommended.
Group B Streptococcus (Strep): is a screening conducted in the third trimester. It is a type of bacteria that is commonly found in the genital and rectal areas of adults. While it’s usually harmless to the carrier, it can pose a risk of infection to newborns during childbirth.
During the screening, a swab is taken from the vagina and rectum to check for the presence of Group B Strep. If the bacteria are detected, it doesn’t mean there’s an ongoing infection but indicates that you are a carrier.
If you test positive for Group B Strep, your healthcare provider will recommend administering antibiotics, usually intravenously, during labour. This is done to reduce the risk of transmitting the bacteria to the baby during delivery, which could lead to infections.
Pelvic exam: may be performed by your healthcare provider to assess the baby’s position in the uterus. This examination involves checking the baby’s head-down position, which is optimal for a head-first delivery.
If the baby is not in the correct head-down position (breech, transverse, etc.), your healthcare provider may discuss ways to encourage the baby to move into the optimal position.
These methods can include exercises, certain positions, or even an external cephalic version, a procedure where the healthcare provider manually attempts to turn the baby from outside the abdomen. It’s an important step to ensure a smooth and safe delivery.
If repositioning the baby is not feasible or successful, your healthcare provider may discuss the possibility of a cesarean section (C-section) with you.
In the third trimester, it’s wise to maintain the caution you’ve practised throughout your pregnancy. This means avoiding things that might pose risks to you and your baby.
In the last few months of pregnancy, it’s a good idea to be careful about long car rides or aeroplane trips, especially after 34 weeks. Airlines might not allow you to board the plane because there’s a small chance of having the baby during the flight.
Sitting for a long time, whether in a car or plane, can make you feel uncomfortable and swollen. If you need to travel, talk to your doctor first, and try to take breaks during the journey to stretch and move around.
As you approach the end of your pregnancy, it’s still okay to exercise, but it’s advisable to avoid working out in hot temperatures. This means skipping activities like hot yoga in favour of staying indoors.
Exercising in the heat increases the risk of overheating and dehydration, which can be concerning during the third trimester. Opt for indoor activities to ensure a safer workout environment for you and your baby.
Continue to avoid strenuous exercises or strength training that could potentially cause injury to your abdominal area. Prioritize gentle, pregnancy-friendly activities and consult your healthcare provider to ensure your exercise routine aligns with your unique pregnancy situation.
Continue to limit your caffeine intake, allowing no more than one cup of coffee or tea per day.
High caffeine consumption during pregnancy has been associated with certain risks, so moderating your intake is a precautionary measure to ensure your and your baby’s well-being.
High-mercury fish, such as shark and swordfish, should be limited due to potential harm to the fetal nervous system. Additionally, avoiding raw or undercooked seafood helps reduce the risk of foodborne illnesses associated with harmful bacteria or parasites.
Unpasteurized dairy products, known to carry bacteria like Listeria, should be substituted with pasteurized alternatives to minimize potential risks.
During pregnancy, it is essential to completely abstain from alcohol consumption and avoid both smoking and exposure to secondhand smoke. Alcohol intake can lead to fetal alcohol spectrum disorders.
Recreational drugs, particularly opioids, pose serious risks during pregnancy. Opioids, including substances like heroin or certain prescription painkillers, can cross the placenta and reach the developing fetus.
In the last few months of pregnancy, it’s a good idea to be careful about long car rides or aeroplane trips, especially after 34 weeks. Airlines might not allow you to board the plane because there’s a small chance of having the baby during the flight.
Sitting for a long time, whether in a car or plane, can make you feel uncomfortable and swollen. If you need to travel, talk to your doctor first, and try to take breaks during the journey to stretch and move around.
As you approach the end of your pregnancy, it’s still okay to exercise, but it’s advisable to avoid working out in hot temperatures. This means skipping activities like hot yoga in favour of staying indoors.
Exercising in the heat increases the risk of overheating and dehydration, which can be concerning during the third trimester. Opt for indoor activities to ensure a safer workout environment for you and your baby.
Continue to avoid strenuous exercises or strength training that could potentially cause injury to your abdominal area. Prioritize gentle, pregnancy-friendly activities and consult your healthcare provider to ensure your exercise routine aligns with your unique pregnancy situation.
Continue to limit your caffeine intake, allowing no more than one cup of coffee or tea per day.
High caffeine consumption during pregnancy has been associated with certain risks, so moderating your intake is a precautionary measure to ensure your and your baby’s well-being.
High-mercury fish, such as shark and swordfish, should be limited due to potential harm to the fetal nervous system. Additionally, avoiding raw or undercooked seafood helps reduce the risk of foodborne illnesses associated with harmful bacteria or parasites.
Unpasteurized dairy products, known to carry bacteria like Listeria, should be substituted with pasteurized alternatives to minimize potential risks.
During pregnancy, it is essential to completely abstain from alcohol consumption and avoid both smoking and exposure to secondhand smoke. Alcohol intake can lead to fetal alcohol spectrum disorders.
Recreational drugs, particularly opioids, pose serious risks during pregnancy. Opioids, including substances like heroin or certain prescription painkillers, can cross the placenta and reach the developing fetus.
Always trust your instincts; if you have any concerns or uncertainties, don’t hesitate to contact your healthcare team for guidance. Regular communication with your provider is key to ensuring a healthy pregnancy.
Labour usually happens between weeks 38 and 41, but it’s hard to predict exactly when. When labour starts, your cervix opens, and your uterus contracts, causing cramps similar to intense menstrual pain. Other indicators of the onset of labour include:
While morning sickness commonly diminishes around the 14th week of pregnancy, it doesn’t follow a strict timeline, and some individuals may continue to experience nausea into the third trimester. It’s normal for pregnancy-related nausea to persist, and in some cases, it might even intensify as your baby grows and occupies more space within your abdomen.
The competition for space among internal organs and the developing baby can contribute to the continuation or exacerbation of nausea during the later stages of pregnancy. If you find the symptoms challenging, discussing them with your healthcare provider can help explore potential remedies or strategies for relief.
During the third trimester, engaging in sexual activity is generally safe as long as it feels comfortable and your healthcare provider hasn’t advised against it. However, it’s advisable to avoid sex if your water has broken, you’ve lost your mucus plug, or if contractions begin before 37 weeks.
If you have any uncertainties or questions regarding sexual activity during this period, it’s essential to discuss them with your healthcare provider. It’s normal for libido to vary during the third trimester, and not feeling like having sex is a common experience.
Pregnancy can bring fluctuations in sexual desire, and these changes are part of the natural course of the journey.
As your baby grows, the available space for movement within the womb decreases, but you’ll still be able to feel their activity. Your baby might be particularly active after meals and in the evening. It’s normal for their movements to change as they adjust to the limited space.
If you ever notice your baby being quieter than usual, a general guideline is to count around ten movements within an hour, which is considered normal. However, variations in movement patterns are common.
If you’re concerned about reduced movement, try consuming something and counting for another hour. If your baby doesn’t reach ten movements within two hours or if you observe a sudden or significant change in their movements, it’s advisable to contact your healthcare provider for guidance.
Regular monitoring of fetal movements helps ensure the baby’s well-being during pregnancy.
As your pregnancy progresses, sleeping on your stomach becomes uncomfortable due to the size of your baby bump. Sleeping on your back for extended periods is not recommended because it may reduce blood flow to your abdomen.
Opting for side sleeping, particularly the left side, with pillows supporting your legs and under your stomach can enhance comfort and promote better circulation.
If you accidentally wake up on your back, simply roll back onto your side to prioritize optimal blood flow for you and your baby.
While there are no guarantees, some generally safe methods potentially encourage labour. Moderate exercise, such as walking, can be beneficial. Engaging in sexual activity may also promote progress; orgasms release oxytocin, which could initiate contractions, and prostaglandins in semen may contribute to cervical ripening. However, it’s crucial to obtain approval from your doctor or midwife before trying any methods.
During the third trimester, engaging in sexual activity is generally safe as long as it feels comfortable and your healthcare provider hasn’t advised against it. However, it’s advisable to avoid sex if your water has broken, you’ve lost your mucus plug, or if contractions begin before 37 weeks.
If you have any uncertainties or questions regarding sexual activity during this period, it’s essential to discuss them with your healthcare provider. It’s normal for libido to vary during the third trimester, and not feeling like having sex is a common experience.
Pregnancy can bring fluctuations in sexual desire, and these changes are part of the natural course of the journey.
As your baby grows, the available space for movement within the womb decreases, but you’ll still be able to feel their activity. Your baby might be particularly active after meals and in the evening. It’s normal for their movements to change as they adjust to the limited space.
If you ever notice your baby being quieter than usual, a general guideline is to count around ten movements within an hour, which is considered normal. However, variations in movement patterns are common.
If you’re concerned about reduced movement, try consuming something and counting for another hour. If your baby doesn’t reach ten movements within two hours or if you observe a sudden or significant change in their movements, it’s advisable to contact your healthcare provider for guidance.
Regular monitoring of fetal movements helps ensure the baby’s well-being during pregnancy.
As your pregnancy progresses, sleeping on your stomach becomes uncomfortable due to the size of your baby bump. Sleeping on your back for extended periods is not recommended because it may reduce blood flow to your abdomen.
Opting for side sleeping, particularly the left side, with pillows supporting your legs and under your stomach can enhance comfort and promote better circulation.
If you accidentally wake up on your back, simply roll back onto your side to prioritize optimal blood flow for you and your baby.
While there are no guarantees, some generally safe methods potentially encourage labour. Moderate exercise, such as walking, can be beneficial. Engaging in sexual activity may also promote progress; orgasms release oxytocin, which could initiate contractions, and prostaglandins in semen may contribute to cervical ripening. However, it’s crucial to obtain approval from your doctor or midwife before trying any methods.
1. Ananth, C.V., Keyes, K.M., Hamilton, A., Gissler, M., Wu, C., Liu, S., Luque-Fernandez, M.A., Skjaerven, R., Williams, M.A., Tikkanen, M. and Cnattingius, S., 2015. An international contrast of rates of placental abruption: an age-period-cohort analysis. PloS one, 10(5), p.e0125246.
2. Bjørklund, G., Chirumbolo, S., Dadar, M., Pivina, L., Lindh, U., Butnariu, M. and Aaseth, J., 2019. Mercury exposure and its effects on fertility and pregnancy outcome. Basic & clinical pharmacology & toxicology, 125(4), pp.317-327.
3. Children’s Wisconsin. Post-term Pregnancy
4. DeSisto, C.L., Kim, S.Y. and Sharma, A.J., 2014. Peer reviewed: Prevalence estimates of gestational diabetes mellitus in the United States, pregnancy risk assessment monitoring system (prams), 2007–2010. Preventing chronic disease, 11.
5. Healthline. Growth Retardation (Delayed Growth)
6 Healthline. Placenta Previa.
7. Johns Hopkins Medicine. Meconium Aspiration Syndrome.
8. Johns Hopkins Medicine. The Third Trimester
9. Kumar, A., Basra, M., Begum, N., Rani, V., Prasad, S., Lamba, A.K., Verma, M., Agarwal, S. and Sharma, S., 2013. Association of maternal periodontal health with adverse pregnancy outcome. Journal of Obstetrics and Gynaecology Research, 39(1), pp.40-45.
10. McQuire, C., Daniel, R., Hurt, L., Kemp, A. and Paranjothy, S., 2020. The causal web of foetal alcohol spectrum disorders: a review and causal diagram. European child & adolescent psychiatry, 29, pp.575-594.
11. MedlinePlus. Premature rupture of membranes.
12. Preeclampsia Foundation. What is preeclampsia
13. Simm, A., 2007. Fetal malpresentation. Obstetrics, Gynaecology & Reproductive Medicine, 17(10), pp.283-288.
14. WebMD. Third Trimester
© Mindsmaking 2024